Prasanna Saligram, Sunita Simon Kurpad, Thelma Narayan
INTRODUCTION
The fifth National Bioethics Conference (NBC) was co-hosted by St John's National Academy of Health Sciences (SJNAHS), Bangalore; Society for Community Health Research Awareness and Action (SOCHARA), Bangalore; and Forum for Medical Ethics Society (FMES), Mumbai which publishes the Indian Journal of Medical Ethics. The conference was held at the beautiful St John's campus, Bangalore from December 11 to 13, 2014, with pre-conference events on December 10, 2014. Since 2005, the NBCs are held once in two years at different venues within India to discuss contemporary and socially relevant issues concerning bioethics. The first NBC was held in Mumbai in 2005. The theme of the 5th NBC was "Integrity in medical care, public health and health research". An international colloquium on "Corruption in healthcare and medicine" took place on the last day. The focus and theme of this conference arose from widespread public perception of corruption in the health sector. Prevailing malpractices have led to a loss of trust and confidence in the health system. This conference aimed to encourage discussion and debate about the role of bioethics as a value base influencing concepts and practice in medical care, public health, and health research. It was hoped that bioethics would evolve not just as a discipline, but also as a widespread movement that effects change.
An Organising Committee, Scientific Committee, Logistics Committee, and the Organising Secretaries, Dr Thelma Narayan from SOCHARA and Dr G.D. Ravindran from St John's worked hard together with Dr Amar Jesani to develop the conference. A secretariat was set up at St John's and a brochure produced. A website was set up for the conference (www.5thnbc2014.org) and two rounds of individual communications went out to all registered participants. A book of abstracts was published and placed in the bag for all participants. Team members from St John's and SOCHARA put in tremendous effort in preparatory work over six months.
PARTICIPATION
The conference was attended by 695 registered participants and many more who came in for individual sessions. Two hundred and fifty were from the student community. These included postgraduates from different disciplines and systems of medicine, community health and theology, and some graduate students. The participants comprised doctors, medical students, social scientists, academics, "bioethicists", counsellors, economists, lawyers, philosophers, journalists, students, theologians, community workers, researchers, advocacy organisations, administrators, and persons from international organisations. The total number of participants across all NBC-related events was over 750 since the conference was open to non-registered participants for specific sessions, including pre-conference events. Participants came from 10 countries – Australia, Egypt, Germany, India, Pakistan, Singapore, Sri Lanka, Thailand, the UK, and USA. From within India, participants from 14 states – Andhra Pradesh, Bihar, Delhi, Gujarat, Haryana, Karnataka, Kerala, Madhya Pradesh, Maharashtra, Manipur, Orissa, Pondicherry, Tamil Nadu, and West Bengal, added richness to the discussions.
PRE-CONFERENCE EVENTS
Three major pre-conference events, outlined below were organised on December 10, 2014.
-
Curriculum development workshop – Bioethics for medical undergraduates
-
Colloquium on the "ethical perspectives in gender in health"
-
SOCHARA meetings around the Community Health Learning Programme (CHLP)
- The annual alumni meeting of the SOCHARA CHLP on December 10, 2014 at St John's enabled alumni to join the NBC. Nearly 50 community health fellows participated from across India, representing the various batches since the CHLP began 10 years ago. They shared their life and work journeys since completion of the fellowship. It provided for richness of experience and also showcased the fact that most were putting into practice what they had learnt during their fellowship. A particular point noted was the connectedness with the communities. The CHLP team of SOCHARA made a presentation of the third phase of the CHLP. A film on CHLP, produced by Krishna Chakravarthy and Abhishek, was shown. Finally, the group met to discuss the ways forward. The opinion was expressed that the meeting was very energising and inspiring. There was a suggestion to form an association. Another suggestion was to form a discussion group to deliberate various issues and also to have internet and social media presence. The efforts of the Madhya Pradesh Fellows to form a Fellows' Collective was lauded. Whether a similar exercise needs to happen in Karnataka and Tamil Nadu was discussed. A small group of fellows came forward to take this discussion and process forward.
- In the afternoon, there was a mentors' meeting of the CHLP. Some alumni have become mentors and hence they participated in the mentors' meeting as well.
- The Academic and Research Council meeting of the SOCHARA School of Public Health Equity and Action (SOPHEA) was also held concurrently.
This workshop was organised by the departments of Medical Ethics and Medical Education from St John's and Christian Medical College, Vellore. The main objective of the workshop was to discuss a draft curriculum and develop it to enhance the process of learning and teaching ethics in medical colleges. The other intermediate objectives were to publish in an indexed journal, the challenges faced in teaching ethics; networking for a continued support for facilitating learning and teaching ethics in medical college, and to develop a resource library to support the process through a sharing arrangement between institutions. The participants were from the medical faculty of teaching institutions and included bioethicists and theologians. Preparatory planning meetings and circulation of documents were done prior to the workshop.
This colloquium was organised to collectively reflect on the ethical perspectives and considerations vis-à-vis gender and to evolve action points to take this forward in health education and research. The axes of ethics in gender that were discussed during the colloquium were – sex selection and gender ratio; gender issues among adolescents; maternal health and reproductive health; domestic violence; and gender issues among women in the health workforce. In her inaugural address, Dr Elizabeth Vallikkad mentioned that this colloquium presents participants from multidisciplinary backgrounds including doctors an opportunity to learn about gender issues in healthcare. Dr Sabu George highlighted the decreasing gender ratio in the country and ethics of female foeticide practised in the country. At the same time he stressed that it is not enough to have a law to prevent female foeticide. Women's empowerment needs to be promoted and this is currently not on the political agenda of the country.
Dr Shaibya Saldanha led a discussion on adolescent issues. She highlighted how the tendency of adolescents is to rebel and that adolescents are only punished for their behaviour. She also mentioned issues around sexuality and how adolescents do not get authentic information regarding this and tend to imbibe the larger societal ways of commodification and violence against women. She stressed the need for adolescents to be taught that they can become adults, without taking risks. Talking about maternal mortality, Dr Evita Fernandes mentioned the term "obstetric violence" and how the medical fraternity is not taught about gender issues in healthcare. This leads to the ethical issues of lack of respect and privacy during child-birth. She highlighted the fact that trained midwives have better sensitivity towards such issues. She outlined measures to overcome "obstetric violence". She mentioned how in Venezuela there is a regulation, passed in 2007, to punish healthcare workers who indulge in "obstetric violence".
On the reproductive rights of women, Deepa from the SAMA Resource Group for Women and Health, Delhi, highlighted how the Bilaspur tragedy where 16 women died during sterilisation was a violation of all reproductive health rights. She also lamented the continued "targeted" approach to family planning and the defeminisation of society. Donna Fernandes from Vimochana highlighted the plight of women subjected to domestic violence and burns. She lamented that the medical system does not take any responsibility to look into the cause of burns and injuries. Registration of FIRs in burns cases is also very low. Of 415 burns cases, only 45 were registered. She stressed the need for a comprehensive approach to issues of domestic violence and burns. The case of women in the health workforce also came up for discussion and how the issues regarding gender in the society gets reflected in the treatment of women members of the health workforce in the country, who comprise a large majority of the workforce but do not have adequate voice.
THE FIFTH NATIONAL BIOETHICS CONFERENCE
Inaugural Address by Rev Dr Paul Parathazham, Director, St John's National Academy of Health Sciences (SJNAHS)
The Fifth NBC was inaugurated by the Director of St John's, Rev Dr Paul Parathazham, a sociologist and researcher of repute. He ended his address with a modified quote of Karl Marx – "Ruling ideas of the time are necessarily the ideas of the ruling class" to the "ruling morality of the time is necessarily the morality of the ruling class". This needs to be challenged and transformed. He also mentioned that social constructions are susceptible to epistemiological constructions. He pointed to the need for an ongoing epistemological critique of ethics with efforts to maximise objectivity.
Inaugural Address by Dr Amar Jesani
Dr Amar Jesani traced the origins of the Forum for Medical Ethics Society (FMES), the organisation which co-hosts the NBC and publishes the peer-reviewed and indexed Indian Journal of Medical Ethics. The existence of FMES and IJME has shown that "a counter-current can become a reality," and "integrity becomes visible when it is challenged and tested." He said the IJME is going through difficult times without funding; as "being a counter-current means that we do not take funds from the pharmaceutical and health industry." The present edition of NBC began with an interaction that he had with Dr Christiane Fischer from MEZIS (No Free Lunch), Germany. Later funding support was organised through MEZIS, SOCHARA, and St John's. He ended his address with an appeal for more concerned persons to rally around IJME to support its existence and added that "morality cannot be left only to the medical profession."
THE PLENARIES
The inaugural plenary set the tone for the conference through two vibrant, thought-provoking and challenging keynote addresses by Dr Shiv Vishwanathan, Professor, School of Government and Public Policy, OP Jindal Global University and Senior Fellow, Centre for the Study of Developing Societies, Delhi; and Dr Farhat Moazam, Professor and Founding Chairperson, Centre of Biomedical Ethics and Culture (CBEC) of the Sindh Institute of Urology and Transplantation in Karachi, Pakistan.
Professor Shiv Vishwanathan spoke of the need for medical ethics to be rooted within a framework of deeper philosophical, sociological and cultural understanding, medical ethics journals can be critiqued as lacking a philosophy. He used a historical lens outlining how "the body" is conceptualised. He proposed that the history of the body be seen as a relation between the body and body politic. The "anatomised, medicalised, and forensic body" as seen during the forced sterilisations of the emergency; foetal destruction and in some aspects of medical practice are linked and yet appear distant from violence and suffering. He pushed further describing the other types of bodies like the objectified body; scientified body ("the invention of the corpse"), the consumerist body; the commodified body; the prosthetic body.
He lamented the militarisation of modern India and used the metaphor of the militarisation of modern medicine and its aggressive approach to the body. He drew attention to the fact that the practice of cosmetic surgery, assisted reproductive medicine and surrogacy has been removed from the ethics of medicine. He threw light on a rapidly growing trend within India with the elderly becoming dispensable and their health problems negating their personhood, e.g. "the father disappears in the disease". He urged the audience to look deeper into the idea of sickness and the definition of disease, and to understand the language of suffering. He suggested that medical ethics and bio-ethics are different conceptual universes.
Professor Vishwanathan said that the theory of rights is inadequate to look at ethics, because it is insensitive to violence and can cause violence. Liberation theology he felt has been more sensitive. He called for a critique of epistemology, ontology, and cosmology before embarking on the introduction of courses in medical ethics. "We can't import medical ethics." We need to evolve and develop medical ethics with a democratic imagination. He mentioned the patient as a citizen needs to be seen as a person of knowledge with their own medical imagination and cultural ideas; and for the doctor/provider to see himself/herself as a tacit constitutionalist listening to the unstated, the silences of life which provide insights into suffering and healing. He strongly urged the medical and medical ethics community to challenge the corrupt practices of the present Medical Council of India and the World Medical Council leadership exposing the current doctor–politician nexus.
In her keynote address, Dr Farhat Moazam took the audience through the history of the evolution of modern medicine, the birth of the "Scientific gaze" and how the Cartesian philosophy brought about a mind–body dualism leading to medicalisation of the human body and the understanding of disease. She challenged participants to question whether it is possible to humanise medicine that is dehumanised. She also brought out the differences between the physician's world as that of working with "objective reality" and the patient's world of "subjective reality". She questioned the myth of an "autonomous", "self-governing" individual and the concept of "informed consent" as an answer for everything in bioethics. She underlined the fact that bioethics is becoming a specialisation rather than a way of doing things and developing and understanding relationships between those who suffer and healers. In her concluding remarks, she quipped that "we fix organs and parts, but the human body and human person is lost."
Felicitations
At the conclusion of the first plenary, the Conference felicitated Professor Farhat Moazam and Professor M Sankaran Valiathan for their lifetime contribution to the field of medical and bio-ethics.
The second plenary was by Dr Anura Kurpad, Professor of Physiology, SJNAMS and Dr Sanjay Nagral, department of Surgical Gastroenterology, Jaslok Hospital and Research Centre, Mumbai.
Dr Kurpad speaking on the topic "Ethics as an essential element in evidence and health policy" questioned the present cereal-centric food subsidies. He brought out the difficulty in putting nutrition on the agenda of commercial crop-oriented agriculture. He also highlighted the setting of unrealistic targets in public policies and the shifting of goal posts. He then outlined the need for concrete practical ethical frameworks to guide public health programmes. He used "The intervention ladder" – From doing nothing to eliminating choice as a way of guiding public health programmes. He ended his speech with a comment – "Hunger is the most political disease."
Dr Sanjay Nagral speaking on the topic "Role of professional councils and healthcare regulators in upholding integrity of medical practice", differentiated integrity as having two dimensions – internal and external. Internal regulations are through such instruments as the Medical Council of India, Indian medical associations, institutional review boards for ethical review of research proposals, etc. Citing certain recent high-profile cases, he mentioned that there have been recent encouraging trends about these processes. But he lamented that some honest practitioners in the medical fraternity have ceded space to the corrupt. External regulation occurs through mechanisms set up by the State with laws, payers (insurance) and community/market mechanisms. He stressed the importance of role models for practice of ethics in medical colleges. Finally, answering the question whether regulation can promote integrity, he mentioned that these can act as reference points for the honest ones; it could generate a fear of punitive action and could be a rallying point for civil society advocacy.
The third plenary was by Dr Ravi Narayan, Senior Community Health Consultant, SOCHARA; Ms N.B. Sarojini, SAMA resource group for Women and Health and Dr Anand Zachariah, Professor of Medicine, CMC Vellore.
Dr Ravi Narayan speaking on "Integrity in public health: systemic challenges and policy paradigms", noted that when it comes to integrity in public health, the choice is clear that of choosing people over markets. He pointed to the ethical issues forewarned in such reports as the ICMR/ICSSR report, Karnataka Task Force Report on Health (2002), etc. He called for action both at the individual level and as a collective. He quoted Atul Gawande's book Better to highlight possible actions that could be taken at the individual level. He drew the audience's attention to the "People's Health Charter" of the People's Health Movement and its expression of collective action. He then pointed to positive developments such as the MPH (Hon) curriculum developed for the Rajiv Gandhi University of Health Sciences, which he termed as "mainstreaming the alternative". He also delineated between two types of professionals – "Activist professional" and "professional Activist" and urged the medical fraternity to choose the former. He also brought out another concept of choosing an appropriate "polypolicy" as against "polypill".
Ms Sarojini, speaking on "Integrity in access to public health services with a specific focus on gender and reproductive health", started with the question, whether women are homogenous? She further pointed to fundamental questions that need to be asked, such as – are women aware of the various programmes? Are programmes reaching them? Which social groups have or lack access? What of quality and privacy? and so on. Public health system neglect has gone on for too long, pushing women to private services. She spoke of the Bilaspur tragedy. She said that this is part of the fundamentalism regarding population control. She dealt with the Bilaspur tragedy in great detail analysing the gender aspects threadbare. She mentioned that honour of the family rests with the bodies of women and marriage. She lamented that right wing politics and right wing economics have come together at the Union level in the country. She also pointed to the risk of losing a lot of ground that had been reached with much struggle. She stressed the need for increased emphasis on strengthening of the public health system and that there is no alternative to that from an equity perspective.
She suggested that some solutions are emerging – to be bold; to engage with difficult questions and contested issues; to work for operationalisation of NALSA – with the Supreme Court of India granting legal status for the third gender and to reach out to old and new friends.
Anand Zachariah, speaking on "Crisis in education of health: ethical challenges in upholding scientific and moral integrity", took up the case of type 2 diabetes as a tracer for his talk. He started with the changed representation of diabetes. Earlier diabetes was diagnosed by the Oslerian symptom base of polyuria, polydipsia and polyphagia. But now the same is done through epidemiological and statistical values with the adoption of new threshold criteria. He mentioned that this has implications in terms of over medicalisation of pre-diabetes. According to the new criteria developed – 50% of adults are pre-diabetic!!
There are deep structural problems associated with the increased diabetic epidemic in the country. He quoted the changed lifestyle and food habits of the urban poor which results in chronic conditions.
The way forward he suggested was to map development vectors against the epidemiological risk factors, adopt a continuum of risk concept approach and so on. He suggested that there is a need to move towards a knowledge of deliberative practice. He further mentioned that ethical knowledge lies in tailoring, translating, and reinterpreting concepts. Textbook knowledge to address the situation of the patient is not enough. He highlighted that the old method of clinical teaching between a mentor and mentee has declined, with computer-based learning and diagnostics leading to a decline in integrity in practice.
The chair of the plenary appropriately summed it up by saying that Dr Ravi Narayan concentrated on the demand side of things, Ms Sarojini on the supply side and Dr Anand Zachariah rounded it up with talking about both the supply and demand side arguments.
The fourth plenary had three speakers – Dr Peush Sahni, Professor, department of Gastrointestinal Surgery and Liver Transplantation, All India Institute of Medical Sciences and Editor, The National Medical Journal of India; Dr Roli Mathur, Scientist D, Indian Council of Medical Research and Dr Nandini Kumar, Former Deputy Director General Senior Grade (ICMR); Dr TMA Pai Endowment Chair, Manipal University; Adjunct Professor Kasturba Medical College, Manipal.
Dr Peush Sahni, speaking on "Scientific misconduct" enumerated the various issues that need to be addressed, namely participants; information and consent; plagiarism, fabrication and falsification; research and writing; publication ethics; authorship, duplicate submission; clinical trial registration; and conflict of interest. He also stressed that ethics or the lack of it has become a major concern with increased instances of scientific misconduct. He also said that there are multiple players involved, namely the researcher, author, reviewer, publisher, reader, etc., and hence the situation necessitates a stringent following of ethics. He highlighted some of the research ethics that need to be considered, namely privacy and confidentiality of patients; informed consent and ethical approval; design of studies and justification for the same; control of data for sponsored studies; and registering clinical trial. Some of the considerations for the ethics of publication would be redundant publication; peer review; and authorship.
Dr Roli Mathur, speaking on "Conflicts of interest", started by listing out the types of conflicts of interest, namely financial and non-financial; institutional and individual; perceived and real. When publishing research studies, disclosure of the sources of funding, sponsorships and possible conflicts of interest is required. There is also a need to explain the methodology and how the ethical guidelines were followed. On the issue of authorship, she mentioned that it should be based on the quantum of contribution made in terms of ideas towards the study. Also important would be to acknowledge the contribution of people who would not satisfy the criteria for authorship. Appropriate credit is to be attributed for information used from other sources. She also drew the attention of the audience to the Vancouver guidelines which outline that all qualified authors should be listed with specific authors taking responsibility for the integrity of the whole. She then enumerated other types of misconduct that can take place, namely, recklessness and negligence; malicious accusations; violations of due process; reprisals against whistleblowers; and cover up misconduct.
Dr Nandini Kumar, speaking on "Research ethics guidelines and regulations for upholding the integrity of research" highlighted the need of the scientific community in India to take the issue of scientific misconduct seriously. She pointed out that some cases of serious misconduct such as plagiarism by prominent scientists in India had unfortunately been treated rather lightly. She emphasised that it was important for the scientific community in India to be aware of legislation such as the Whistleblowers' Protection Act which could be used to point out cases of misconduct.
The fifth plenary was an "International symposium on corruption in healthcare and medicine". The speakers were Dr Sujatha Rao, Former Union Principal Secretary, Health, India, IAS (retd); Dr Peter Mansfield, General Practitioner, Australia and founder Healthy Skepticism. The session started with the launch of the fourth Global Health Watch report produced by the People's Health Movement (PHM). The report provides a critical analysis of health-related issues and policies (available on www.phmovement.org).
Dr Sujatha Rao talking about "Corruption in healthcare" mentioned that after the revenue and police departments, the health department is the most corrupt. She also mentioned about corruption getting a mention in a TV series "Satyameva Jayate" and also the recent BMJ publication on cutbacks and corrupt practices in medical care in India. She recalled how National Rural Health Mission funds were siphoned off in Uttar Pradesh for which the State Health Secretary was sent to jail and the Health Minister had to resign. She mentioned the abdication of the regulatory role by the health system. She lamented the politicisation of a professional body, the Medical Council of India. She also mentioned that regulatory capture happens in the name of stakeholder consultation. She advocated for a strong public health law that governs both the public and private sectors in medical care.
Peter Mansfield talking about Temptation and biases in the context of the pharmaceutical industry and the links with the medical profession and ethical medical practice, explained that intended errors are temptations and unintended errors are unintended biases. He highlighted the use of metaphors as being very powerful. He also mentioned that this was one of the main reasons why Healthy Skepticism was started (www.healthyskepticism.org). He also mentioned that it is the systems to be blamed rather than the individual for the malaise afflicting healthcare. He said that if one puts a good person in a wrong system, the wrong system would win hands down. He also joked that small gifts are cost-effective for the companies.
The final plenary titled "Just a gift?" highlighted the influence of pharmaceutical marketing activities on prescription behaviour. Christiane Fischer from Germany mentioned that there were 50,000 doctors and 15 million pharmaceutical company representatives in Germany. At the same time there was a suggestion that beyond the demonisation of the pharmaceutical industry, one needs to start engaging with the industry, getting them to the table, and holding them accountable to a code of conduct. One should try and bring the medical representatives on board as well.
PARALLEL WORKSHOPS AND ORAL PAPER PRESENTATIONS
These were organised under four broad themes – research ethics; clinical ethics; public health ethics; and cross-cutting themes. An outline of the discussions is given below:
I RESEARCH ETHICS
Informed consent – A session on the integrity of informed consent looked at the ability of women seeking maternal or child health services in public hospitals in India to make decisions about research participation, and found them vulnerable to coercion. One way the study circumvented this problem was to give the option of refusal or an opt-out clause after the interview process.
Authorship – On the issue of authorship, ICMJE has included four criteria for authorship and one of the criteria defines honorary authorship. This was found to be the most abused. Indians indulged in this more frequently. The honorary authors were the head of the departments and seniors. The most common form of contribution cited was proofreading and statistical analysis. "People who are aware of honorary authorship indulge in it." The traits of good authorship practices were brought out through two case studies of unethical authorship. The issues of plagiarism, conflict of interest, publication bias, and authorship were discussed.
Conflict of interest – The issues surrounding conflict of interest (COI) was taken up in another session. There was a general discussion on what constitutes COI. The four A's of managing COI, namely awareness, assessment, acknowledgement, and action were discussed. The problematic physician–pharmaceutical industry nexus influencing prescription behaviour was brought out. Continuing with the pharmaceutical industry and the role of regulation, the dialectic relationship between governmental and self-regulation was debated. The pharmaceutical industry has its own code of conduct which is frequently violated raising the issue of efficacy of self-regulation and hence whether governmental control could be the way to go. The ethical issues that intellectual property rights (IPR) bring out for ensuring access to medicines was presented. Some of the suggestions that emerged were to bring these issues to college students. There was also a suggestion that to overcome problems posed by IPR, there is a need for neutral institutions to undertake research. Pharmaceutical companies can contribute to a fund that helps finance such bodies. However, the ethical dimensions of this arrangement need to be carefully thought through.
Institutional ethics committees – On the institutional ethics committees (IECs), of the 22 IECs studied in Mangalore, only 26% of the IECs were registered. There were problems of representation. The suggestion that came up during the discussion was that EC/IRB members should be made to understand the criteria and there must be FRCAP/AHAP for accreditation. One of the action points that emerged was to minimise the risk of coercion in healthcare research.
Knowledge, attitude and practice – A study on knowledge, attitude and practice (KAP) about research ethics and clinical trials was presented. The study revealed that the researchers knew at least one instance of inadequately explained consent documents, forged number of study samples; adjusted data and offering guest authorship indicating a larger malaise existing within the research community. Some suggestions that emerged from the session were to organise research methodology classes during postgraduate teaching programmes; arranging refresher courses; and orienting and sensitising researchers about patients' concerns.
Human embryonic stem cell research – The ethical dilemmas that human embryonic stem cell research presents were debated. That the scientists prefer embryonic stem cells as against adult stem cells further compounds the situation. Also, the destroying of the extra embryos that are produced during in-vitro fertilisation (IVF) poses further ethical questions about the beginning of human life. The presenter argued that human life begins at conception itself. The argument that IVF embryos which are orphaned anyway would die and hence could be used for research was countered.
Audio-Visual recordings of informed consent – Audio-visual (AV) recordings of the informed consent is a new phenomena necessitated by the new regulations that have been brought in the country. There was a preliminary study of the experiences with the AV recordings and it was found that there was an overall positive response to this from researchers. On the other hand, patient trust had increased.
II CLINICAL ETHICS
Ethics of care – The dilemmas of confidentiality, boundaries competence, and emotional experiences for health professionals were brought out. There was an overall consensus that professionalism should not override humanitarian concerns. The dilemma was raised of nurses regarding palliative care where the patients prefer home or hospice as their place of care and sometimes refuse treatment but at the same time families do not accept the financial burden or care-giving burden. The solution discussed was about effective communication with family members. In the case of multidrug-resistant tuberculosis (MDR TB), the question was about what death means to health professionals? The need for a holistic support system was highlighted. There was also an urgent need for a fundamental shift from the industrialization of healthcare. "The new normal" of the return on investment (ROI) driving healthcare was presented. The action point that emerged was to impart values among medical graduates as it was appreciated that change cannot come overnight.
Ethics of disclosure – Ethical dilemmas arising in the context of imparting psychoeducation to a professional were discussed. The four principles do not always provide answers. There have been cases where the mental illness of the bride is hidden before marriage, for fear of stigma. The fact that the use of public health research data fosters transparency, avoids duplication but can be misused. Some of the barriers identified were the limited precedence, confidentiality, and trust. The dilemma of "Does science benefit or the patient benefit?" was discussed and the question was that if the patient is not benefiting; should it be disclosed or not. Disclosure has an important role. It was agreed that it is a process in evolution. There was a hope expressed that in five years, more questions may be answered.
Stored samples of stem cells – In a workshop on stored samples of stem cells, it was discussed that the clinical data of the stem cells are available only at presentation and lost for follow-up. That the ethical aspects are still nebulous was brought out. The Unesco declaration that the "owner should share the benefit" was highlighted. There was a question raised whether IEC approval helps, to which there was a consensus response that there was no harm in following informed consent as a mark of respect to the patient, and confidentiality and anonymity was to be maintained. Ethics around the issues of ownership of body tissue; custodianship; transfer; commercialisation are to be borne in mind. A reflection from the rapporteur was that the discussion being too "medicalised".
Over-diagnosis – The harmful unnecessary treatment, needless suffering and high costs resulting from over-diagnosis were highlighted. There are various categories of people involved in over-diagnosis – doctors; patients; hospitals; media; industry and others requiring a response at multiple levels. Some possible action points discussed included evolving monitoring mechanisms; and a look at some of the recent experiments like the AIIMS implementing a crackdown on over-diagnosis and battery tests through the Society for Less Investigative Medicine (SLIM) initiative.
Clinical ethics committees (CEC) – The different roles between IRBs and CECs with the former being responsible for review of research proposals and the latter for clinical ethics were discussed. The paternalistic nature of the doctor – patient relationship in which the doctor has to make personal decisions for patients is increasingly burdensome. Doctors need support from a body when making difficult decisions and in this the CECs can help. Also discussed were the auditing of CECs and whether the dissenting notes need to be carried forward.
The need for boundaries – A workshop explored the meaning and need for boundaries in the healthcare professional-patient relationship through discussions and use of clips from films. The role of context in differentiating an acceptable "boundary crossing" from an exploitative "boundary violation" was discussed. The harm that occurs due to both non-sexual and sexual boundary violations was emphasised. Various scenarios were discussed to enable health professionals to prevent/deal with boundary issues in clinical practice. The questions raised by the members of the audience provided an opportunity to clarify some important myths- –such as ensuring boundaries in clinical care does not mean that it is a cold impersonal relationship – rather it ensures a safe framework for a warm and empathic health professional–patient relationship.
III PUBLIC HEALTH ETHICS
A discussion was started on how public health ethics informs the health crisis perpetrated by certain forms of development like the extractive industries. The values underpinning public health ethics such as equity, solidarity, social justice, etc., help in such circumstances. The rapporteur reflected that rights were not listed as part of public health ethics.
Financial inclusion – The importance of financial inclusion as an ethical imperative for various benefits to reach the marginalised was asserted. However, it was highlighted that most women who qualify for benefits through various social programmes do not have the required bank account in their names, and are deprived of these benefits.
Screening – Regarding the dental screening, it was reflected that often no value is added due to this, as patients may already know about their dental condition. Private medical colleges which have mushroomed are looking for cases, and often leaving the patients with large bills. There has been a problem with follow-up after camps. Concern about ethical implications of technology in screening programmes using examples of ultrasonography (USG) in pregnancy, breast cancer screening were expressed. Also emphasised was the importance of costs not falling on patients due to this screening.
Polio eradication campaign – The ethics of the polio eradication campaign (Odisha case study) was explored through data from newspapers, archives, and interviews. Various technical and anthropological dimensions of the programme were discussed. Challenges of implementation in tribal areas were discussed where people were demanding for services other than polio drops. There was a perception that the drops were harmful, and some that it has to be taken only on specific days (based on the programme days). Concern was expressed that due to the polio immunisation campaign, the other public health interventions are getting ignored. The low emphasis on health determinants was also highlighted, besides inadequate involvement of doctors (though it was pointed that some doctors in peripheral areas do selfless work). The growing trend of lower middle class women opting for an hysterectomy to get rid of the "trouble" of the uterus got a mention.
Occupational health – The dual loyalties of the occupational health (OH) physician was presented, where in the main obligation of the physician is to protect worker's health but is paid by the management. It was also highlighted that the code of OH ethics has expanded the definition of OH to include the health conditions of the communities surrounding the industry. Some of the issues discussed pertaining to the OH were:
- Applicability of the OH laws for unorganised labour
- Applicability of the OH laws for the downstream/outsourced processes
- Corporate social responsibility (CSR) as a vehicle to improve OH
- Impact of dilution of labour laws on OH
- Grievance redress mechanisms for workers
- Mental health dimensions of OH
IV CROSS-CUTTING THEMES
WHO session on integrity and corruption in healthcare – Transparency and integrity in the provision of healthcare and in the pharmaceutical sector are key concepts in public health ethics. Corruption decreases the funds that are effectively available for public health programmes and medicines, and a high level of unethical practices has been shown to have a direct impact on health outcomes. This is why tackling these practices is of crucial importance, and WHO has had long-standing programmes in this area.
This session explored the concepts and modalities of transparency and integrity, and how they can lead to improvements in inefficiencies in healthcare. It provided an overview of WHO's activities, as well as perspectives from Singapore, India, and Thailand illustrating the relevance of the issues at the country level, and recommended best practices on how to address corruption in the health sector. The experience of Thailand and Singapore in promoting good governance for medicine (GGM) at the national level was shared with outcomes and impacts after introduction of the WHO GGM and its operating framework. In Thailand this included the development of policy guidelines; national networking; an information database; dissemination of ethical practice information and assessment. It resulted in a better drug procurement and management system; mechanisms for transparency; participatory and consultative processes. The case of Singapore where the physician prescribes and dispenses drugs was highlighted. The laws place a huge onus on physicians to follow ethical practices. The fact that Singapore also uses multi-pronged approach to drug regulation was also brought out. The crucial aspect of bringing in transparency for improving accountability was highlighted. It was hoped that India could move from micro- and state-level initiatives to a larger national-level approach in this regard.
Corruption in healthcare research – The following forms of corruption were discussed: payments for drug approval, plethora of regulations, and cumbersome procedures. There was also a debate whether corruption was more widely practised in AYUSH or allopathy? Private or public? It was pointed out by participants that corruption was greater in AYUSH! The necessity of the students needing role models for ethical practice was highlighted. A change in the practice of corruption cannot be brought about merely through individual change alone. A larger policy and system change was needed. It was noted that globalisation is leading to an accentuation of profit motivation leading to human rights violations and unethical practices. The ethics of the revolving door of regulation was discussed. While generally corruption in the public health system always comes to the limelight, there are more corrupt practices happening in the private sector.
Towards a solution – A workshop was held to come up with solutions for preventing corruption in healthcare and some of the actions that emerged were to start teaching ethics to young doctors. Another action was to pursue legal activism and to look for enforcement of rules. There was also a proposal to evolve a people's forum for tackling issues in healthcare. A regular monthly monitoring session and wide publicity on the issues within India were some of the other suggestions that emerged.
Gender – In the case of surrogacy and assisted reproductive technologies (ART) it was noted that women were neglected with little access to care after the completion of the surrogacy – "Forgetting the boatman after crossing the river." With surrogacy and ART, reproduction has been brought into the market. The workshop reiterated that the group was not anti-technology but concerned about the intersection of technology, patriarchy, and reproductive care. The caste factor in surrogacy was brought out.
On sexual violence, issues of confidentiality and autonomy of the person who has suffered sexual abuse and the dilemma faced by the counsellor who has the primary duty to report to the concerned authorities were brought out. Sexual violence has both physical and mental health implications. The need for such issues to be addressed as part of the Protection of Women against Domestic Violence Act (PWDA) was expressed. Also expressed was the need for addressing the multiple pathways of perpetration of domestic violence.
Watching ethics – The workshop described how a discourse into bio-ethics was initiated by a foray into film-making and showed how this can be a powerful teaching tool even in resource-poor situations. The rich experience of the facilitators of the workshop highlighted the wide array of bio-ethical themes which can be addressed by effective use of videos. The workshop stimulated the audience to consider developing their own productions.
Ethics of digital media – In the workshop on the ethics of digital media, there was an exercise in which various scenarios were given to the participants such as the photo of patient, checking drug information online, posing for a "selfie" before entering the operation theatre (OT), tweeting about medical malpractice, and so on. There were many grey areas identified and hence the need for such a workshop. Social media further adds to the dilemma. Some of the steps proposed for ethical decision-making were to think through who will be affected by the decision; review of the ethical and legal standards for this; biases to be considered and if available take alternative course of action.
POSTER PRESENTATION
The poster session saw several posters being displayed and an appreciative audience weaving their way through them and asking questions. A wide range of themes were covered.
One poster traced the historical journey of the discourse of medical ethics in medical education in India and noted that despite some 100 years after the Indian Medical Act, little has been done to date to bring medical ethics into the medical curriculum. Another poster debated the ethics of introduction of genetically modified food crops into the Indian market without a proper ethical enquiry into the various factors involved such as actual benefits, risks to consumers and long-term economic impact on farmers. A poster on 'Plagiarism and use of software', which could be used to screen publications and theses, sensitised both students and teachers in the audience on this important issue. Another poster debated the ethics of the continued use of OPV (oral polio vaccine) in view of the risk (albeit low) of vaccine-induced paralysis. Other immunisation options were highlighted. Another poster discussed the knowledge, attitude and perception of doctors and patients regarding the principles of bio-ethics. One poster discussed that while biomedical Indian journals had improved in their information/instructions to authors, several journals needed to ensure better compliance by authors to promote ethical research and publications. Another poster recounted the practical challenges faced by a psychiatrist while trying to uphold a patient's right to confidentiality and the need to protect rights of patients, family members and even the treating doctor. A poster outlined the effective sensitisation of intern doctors to ethical issues in doctor patient relationship by using a 4-hour interactive session followed by testing using an OSCE format.
PARALLEL ARTS FESTIVAL
One of the unique features of the conference was the parallel arts festival held during the duration of the conference organised by the Division of Health and Humanities, St John's Research Institute together with "Empathise Now!". Powerful films were screened during the conference. There were plays specially scripted and developed for the NBC enacted around the theme of empathy. Two medical students curated an exhibition of newspaper cuttings around the theme of integrity in the health profession aptly named "Heal thyself". A great attraction was a very meaningful "dolls exhibition" where hand-made dolls enacted scenes from daily life depicting the life situation of the social majority by Francoise Bosteels. More than 100 hand-crafted dolls were on display on the various themes around the medical profession.
CONCURRENT EVENTS
During the conference two concurrent events were organised. On December 12, 2014, the Forum for Medical Ethics Society (FMES), held its annual general body meeting. A few new members joined the Forum and took organisational responsibilities.
Another concurrent event the same evening was a meeting of the international People's Health Movement (PHM). PHM members from Sri Lanka, Germany, India, and the UK participated sharing their activities. During this meeting, the Global Health Watch – 4, the alternative World Health Report was also discussed.
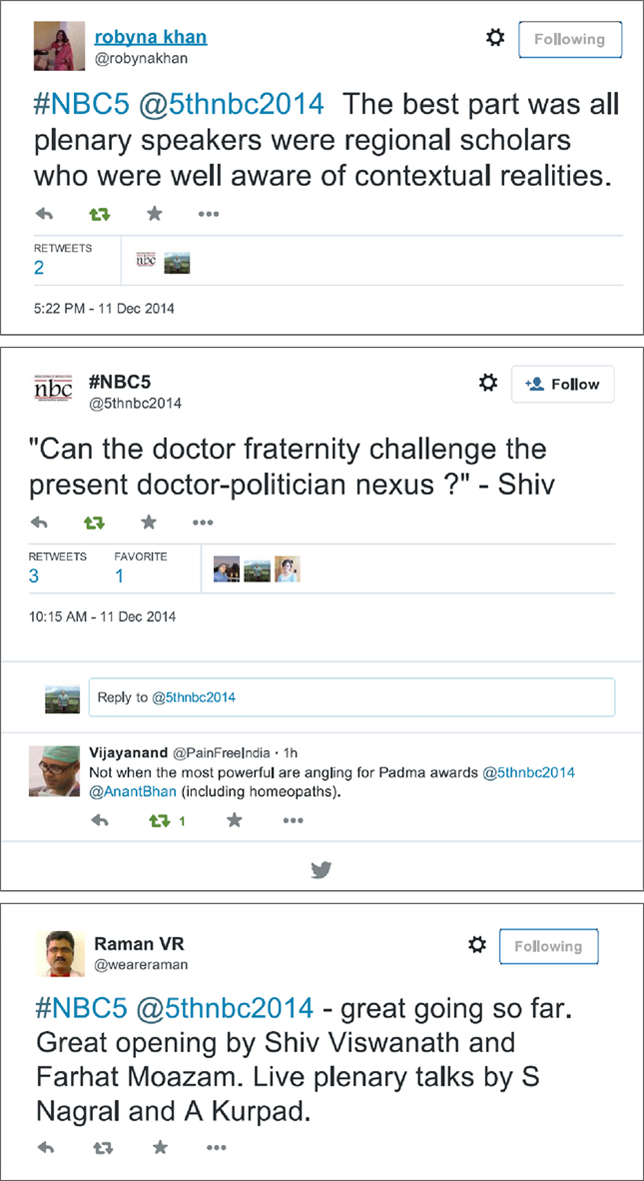
MEDIA AND SOCIAL MEDIA
The media was creatively used to highlight the issues covered during the conference. There was a pre-conference press meet organised to publicise the event and the conference was also covered in Indian and German newspapers. For the first time, social media was used actively during the conference on Facebook and Twitter. Conference participants actively tweeted during the sessions and nearly 80 tweets were put up. At the same time, some of the discussions were put on the Facebook account as well.

CONCLUDING SESSION
In the concluding session, Dr Sunita Simon Kurpad from SJNAHS; Dr Anant Bhan from FMES, and Mr Prasanna Saligram from SOCHARA presented a summary of the conference based on the notes taken by a reporting team. They encapsulated the key issues and events, and highlighted the main messages and action points that emerged during the plenary sessions, paper presentations, and workshops. Finally, Dr Amar Jesani from FMES; Dr Christiane Fischer from Mezis; Dr Thelma Narayan from SOCHARA; and Dr G.D. Ravindran from SJNAHS reflected about future action. Dr Amar Jesani noted that this was the biggest bioethics conference that was held in the last 10 years. He recollected how in the 1980s nobody would talk to him. This conference has changed the situation for IJME not just in terms of money, but in terms of interest and commitment generated among participants for bioethics. He suggested that one needs to reach out to mainstream organisations/institutions and hospitals between conferences.
Dr Thelma Narayan mentioned the need for further discussion and work around social science and public health ethics including research. She hoped that the formation of a Bangalore Bioethics Forum would emerge from this NBC. Based on the workshop organised by WHO, she pointed to the need to explore the possibility of setting up of a high-level national bio-ethics commission as has been done in other countries. This would be similar to the National Human Rights Commission and the National Commission for Women. Dr Christiane Fischer mentioned that corruption was a global problem. She called for the creation of "ethical medicine" as a counter to "unjust medicine". Dr G.D. Ravindran pointed out the efforts put in by various organisations which made the conference a huge success and thanked each and every person who contributed towards the Fifth NBC. A lot of voluntary work has gone into the preparatory work and the conduct of the Fifth NBC and the efforts made by every volunteer and participant were appreciated.
Donor partners who have provided solidarity and support for the conduct of the Fifth NBC were thanked. These include:
Indian Council of Medical Research (ICMR), Delhi; Medical Council of India (MCI), Delhi; Sir Ratan Tata Trust (for participation of alumni and fellows of the SOCHARA CHLP); Sudha Memorial Trust, Bengaluru, India; Bread for the World, Germany; Misereor, Germany; David and Lucille Packard Foundation; USA; Foundation for Promotion of Open Society, USA; Wellcome Trust; UK; and other donors.
ACTION POINTS FOR THE WAY FORWARD
This time, for the conference, all presenters were urged to reflect upon and identify some action points for the ethics movement. Accordingly, several suggestions were made from different viewpoints. There is a need to develop a deeper understanding of the philosophy underlying medical ethics from a sociocultural perspective. Institutions can impart values among young graduates studying health science through role models, good practice, reflexivity and systematic training through curriculum development for medical ethics. India needs to develop and adopt a national public health law. The campaign to prevent over-diagnosis such as the Society for Less Investigative Medicine (SLIM) group that has emerged in AIIMS can be spread. We can look beyond the demonisation of the pharmaceutical industry through engagement and bringing the medical representatives on board. There was a suggestion that the NBC needs to send a strong message that the government should work towards accountability in the Central Drug Standards Control Organisation (CDSCO). It was also suggested that community monitoring and planning for health could bring in social accountability and reduce corruption. Information and communication technology (ICT) enablement could be one solution for mechanisms to bring in greater transparency and accountability. On the issue of assisted reproductive technology (ART) and surrogacy a new ART and Surrogacy Bill is being formulated and it was felt that advocacy is required around this and a need to engage in the above was expressed. Advocacy is required to introduce outpatient clinics for OH conditions in government health services.
CONCLUSION
The fifth NBC was a memorable experience, bringing together diverse groups of people to reflect together on ethical issues concerning medical care, public health, and health research. The rich mix of plenary sessions, paper presentations, workshops, films, posters, plays, and dolls' exhibition allowed everyone to participate. Several challenges were voiced with difficult questions raised. It is up to the participants and organisations to respond and take the movement for ethical healthcare forward. The energy generated will certainly help in taking forward the discipline and the movement for bioethics.
| About the Authors |
Prasanna Saligram
Society for Community Health Research Awareness and Action (SOCHARA)
Sunita Simon Kurpad
Professor, Departments of Psychiatry and Medical Ethics
St John's National Academy of Health Sciences, Sarjapur Road, Bangalore, 560 034 INDIA
Thelma Narayan
Society for Community Health Research Awareness and Action (SOCHARA)