RESEARCH ARTICLE
Voluntary and rights-based family planning for women: Observations from a community-based study in southern India
SHRUTHEE SG, SENTHIL ARASI, SEENIVASAN P
Published online first on February 12, 2025. DOI:10.20529/IJME.2025.010Abstract
Background: Family planning programmes globally emphasise voluntarism and rights in contraceptive provision, shifting the focus away from fertility regulation. With the intent of measuring the policy-practice gap, this study aims to determine access to voluntary rights-based family planning services among women of reproductive age.
Methods: Between November 2018 and January 2019, 390 married women aged 18 to 44 years residing in Kanchipuram, Tamil Nadu, were interviewed, after obtaining written informed consent from the participants. Agreement between intended and actual family size and spacing, perceived informed choice and contraceptive coercion during client-provider interaction were the primary outcomes studied. Univariate analysis using Pearson’s or Trend chi square tests and multivariate logistic regression were used to analyse the factors associated with contraceptive coercion; adjusted odds ratios (AOR) with their 95% confidence intervals are reported.
Results: Of the 390 most recent pregnancies, 114 (29%) were found to be unintended. Reported concurrence of intended versus actual family size and spacing among respondents was 76% (118/155) and 42% (121/287), respectively. During interaction with a healthcare provider, only 139 (36%) were offered a choice of two or more modern contraceptives; others were advised either tubectomy (69, 18%) or intrauterine devices (IUD) (50, 13%) as the sole option. In the past five years, 181 (46%) women reported adopting a modern method voluntarily, while 33 (8.5%) were forced and 8 (2.0%) were coerced to use modern contraception. Multivariate analysis revealed that women’s employment status (AOR: 13.1[1.3,127.6], P=0.027), public healthcare facilities (AOR: 18.7 [1.8, 193.2], P=0.014), and long-acting reversible contraception (AOR: 30.5 [8.2, 112.6], P <0.001), IUD in particular, were strongly associated with contraceptive coercion.
Conclusion: Provider bias and coercion to use selective modern methods in a limited contraceptive choice setting leaves much to be desired. Expanding the basket of choices and mainstreaming indicators pertaining to informed decision making and rights-based care is imperative.
Keywords: coercion, contraception, family planning, informed choice, voluntarism, reproductive rights
Introduction
Following the consensus arrived on at the International Conference on Population and Development (ICPD) in 1994, there was a marked shift in the policy mandate of family welfare programmes worldwide, from a target-oriented approach which focused on population stabilisation, to a person-centred approach towards family planning based on individual rights [1]. It brought the realisation that empowering women with the knowledge and agency to control reproduction, and providing access to their contraceptive method of choice is one of the most cost-effective solutions to achieve gender equality which is one of the Sustainable Development Goals (SDG) [2]. SDG target 5.6 and indicator 5.6.1. focus on women’s ability to make autonomous choices over their sexual and reproductive health [3].
As per the Family Planning 2030 initiative, voluntary rights-based family planning is a programmatic approach that aims to uphold individual rights in deciding “whether, when and how many children to have”; to equip individuals and society with the required sexual and reproductive health information and services, and to enable them to access these services “free from discrimination, coercion and violence” [4]. The available evidence suggests that only 56% of married women are able to decide freely about their sexual and reproductive health and rights (SRHR) [5]. A family planning programme that is not rights-based would fail to achieve the desired reduction in the unmet need for contraception. The consequences that would follow are unintended pregnancies and avoidable reproductive morbidity and mortality [6].
Globally, 48% of all pregnancies are unintended, representing 121 million pregnancies each year between 2015 and 2019, with India contributing 18% of the burden [7]. With India having nearly one-fifth of women aged 15 to 49 years worldwide, the fertility status of women in India has a long-term demographic significance. In any case, ensuring human rights in the provision of contraceptive services is a moral imperative; not merely a value addition [6]. While the official policy of family planning programmes is to advocate for informed choice and thereby encourage voluntary adoption of contraception, the surprisingly thin base of evidence available on this subject indicates that these mandates are rarely followed in practice[8]. Hence, in our study, we aim to determine access to voluntary rights-based family planning services among married women of reproductive age and to analyse the barriers to access from a socio-cultural and healthcare perspective.
Methods
The present study was conducted to fulfil part of an MD dissertation entitled “Person Centred Care in Family Planning among Women in Kanchipuram, India – A community based cross-sectional study” [9]. The study was conducted in the field practice area of Mangadu Primary Health Centre (PHC) in Kanchipuram, Tamil Nadu, which is the southernmost state of India. Mangadu is a town panchayat located in the sub-urban belt of Chennai. Between November 2018 and January 2019, 390 resident married women in the reproductive age group (18 to 44 years) who were pregnant at least once in the preceding five years, irrespective of the pregnancy outcome, were interviewed for the study.
Considering that 46.4% of the participants in this study, with a perceived need to delay or limit pregnancy, had adopted contraception voluntarily, the minimum sample size with adequate power to estimate the above proportion with an absolute precision of 5% at 95% confidence level was found to be 382; hence the sample of 390 women was deemed sufficient for the purpose of the present study. All five health subcentres (HSC) of the Mangadu PHC were sampled in proportion to population size to minimise selection bias, as each HSC has a designated female multipurpose health worker providing outreach contraceptive services. Two to four Anganwadi centres (AWC) were randomly chosen from each subcentre as required, and starting at a random point, consecutive houses with eligible participants were sampled from the catering population till a maximum of 30 participants were sampled under each AWC or till sample size required from that subcentre was reached, whichever came first.
The data were collected by administering a structured questionnaire in the local language through personal interviews at the participants’ homes. Intra-household decision making dynamics with regard to family planning, contraceptive awareness and ever-use was assessed among all study participants. Among users of any modern method in the past 5 years, women’s experiences with family planning care at any healthcare facility including range of contraceptive services offered, perceived informed choice and contraceptive coercion were studied. Modern contraceptive method is defined as “a product or medical procedure that interferes with reproduction from acts of sexual intercourse”. This terminology excludes traditional contraceptive methods which are based on fertility awareness and periodic abstinence. Ever-use refers to self-reported use of a modern contraceptive method at any time, including current usage; while recent use is operationally defined to indicate start of most recent episode of use in the preceding five years[9]. “Forced contraception” is said to occur when a woman is given contraception without her knowledge or consent. “Coerced contraception” is said to occur when misinformation, or intimidation is used to compel an individual to accept contraception; or when access to benefits or services such as termination of pregnancy are made conditional on acceptance of contraception [6]. Contraceptive coercion is used as a blanket term to refer to occurrence of either coerced or forced contraception.
Descriptive statistics, namely frequency for qualitative data and mean [standard deviation (SD)] or median [interquartile range (IQR)/range] for quantitative data are used as appropriate. Sociodemographic and healthcare related factors were analysed for association with access to voluntary family planning using Pearson’s or Trend Chi square tests. Binomial logistic regression was performed to ascertain and predict the strength of association of contraceptive coercion with statistically significant factors identified by univariate analysis, and other contextually relevant factors; adjusted odds ratios (AOR) with their 95% confidence intervals are reported. A p value <0.05 was considered to be statistically significant. Frequency of missing data was less than 5% for all critical variables; hence pairwise deletion was adopted during analysis. All statistical analyses were performed with SPSS (version 23; SPSS, Inc., Chicago, IL, USA).
Approval was obtained from the Institutional Ethics Committee of the government-run Stanley Medical College, Chennai, and written informed consent was obtained prior to the study from all study participants.
Results
Socio-demographic profileThe target population was married women aged between 18 and 44 years; however the age distribution of the 390 participants in the study ranged from 19 to 40 years with a mean (±SD) age of 27 ± 3.8 years, as eligible participants were required to have had a pregnancy in the past 5 years. Four (1%) women were illiterate, 84 (22%) and 209 (53.5%) had completed at least 5 and 10 years of schooling, respectively; while 93 (23.5%) participants were graduates. The percentage of working women in this population was low (12%) with a median (IQR) individual monthly income of Rs 7000 (3750–10000). A sizeable majority (302, 78%) were Hindus by religion, with 39 (10%) and 48 (12%) being Christians and Muslims, respectively.
The mean age at first marriage and first conception was 21 ± 3.2 years and 22 ± 3.2 years, respectively. While 27 (6.9%) women were married before the legal age for marriage of 18 years in India, 20 (5.1%) women reported teenage pregnancies. The minimum and maximum age at first conception was 13 and 36 years, respectively.
Unintended pregnancyTill date, 303 (77.6%) women reported two or less pregnancies; 69 (17.8%) reported three pregnancies, while 18 (4.6%) had four or more pregnancies. The median (range) number of pregnancies per woman was 2(1-15). With respect to the 390 most recent pregnancies occurring within the preceding five years, 276 (70.8%) were intended, while 114 (29.2%) conceptions were unintended. Of the 114 unintended pregnancies, 29 (7.4%) pregnancies had been conceived when no more children were desired (unwanted) and 85 (21.8%) pregnancies occurred earlier than desired (mistimed).
Desired vs completed family sizeThe desired family size ranged from one to four children, with a majority (329, 84%) desiring two children. The number of actual living children ranged from zero to six, and the mean completed family size was 2 ± 0.6 among sterilised couples. At the time of the study, 46 (12%) women had more living children than intended, and only 32 (69.5%) of them had undergone sterilisation. The reasons cited for having more than the intended number of children included unwanted pregnancy (14, 29%), son preference (12, 26%) and familial pressure (12, 26%). Among the 155 women who had completed their family size at the time of the study, there was 76% (118/155) concordance between the intended and completed family size.
Desired vs actual spacingDesired spacing between consecutive pregnancies ranged from 1 to 7 years in the study population with the median (IQR) being 3 (2–4) years. With 292(75%) women conceiving within one year of marriage, the median (IQR) spacing achieved by newly married couples for their first child was 4 (2–12) months. Whereas for subsequent pregnancies, the median spacing achieved was 27 (18–40) months. Among the 287 women who had had more than one pregnancy at the time of the study, only 121 (42%) women had achieved their reported desired spacing in their most recent pregnancy.
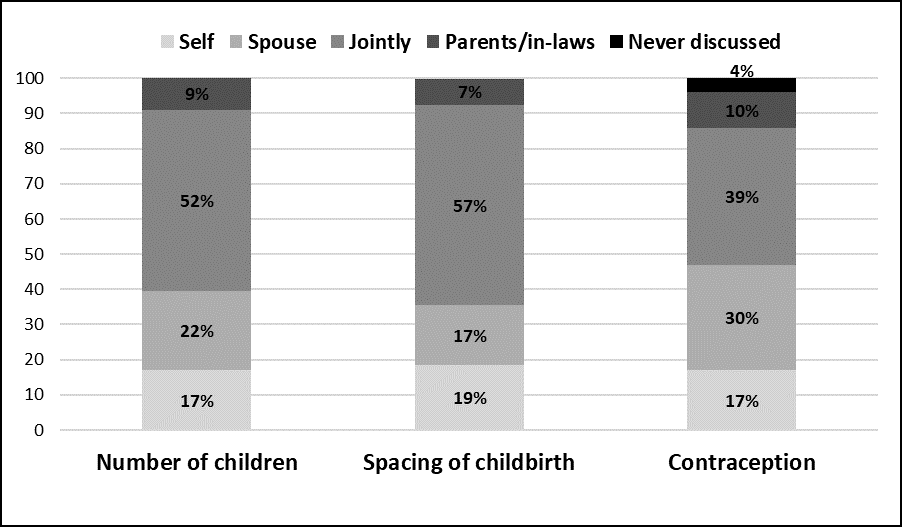
Intra-household decision makingNo more than 168 (43%) women acknowledged being the principal decision makers when it came to their own healthcare; while 64 (16%) women reported making decisions jointly with their spouse, 158 (40%) women had decisions made for them by either the spouse (155, 37%) or the parents/in-laws (5, 3%). Seventy-one (18%) women reported that they were not allowed to go to a healthcare facility without being accompanied by a family member. Regarding family planning, 312 (80%) women reported freely communicating with their spouse. The role assumed by the woman, her spouse and parents/in-laws in the decision making related to family planning as reported by the study participants is given in Figure 1.
Figure 1. Primary decision maker at household level in various domains of family planning (n=390)
Regarding method acceptance, sterilisation was considered essential by a greater proportion of women (350, 90%) and their spouses (359, 92%), as compared to reversible methods (129, 33%) and (152, 39%), respectively. Nineteen (4.9%) and 199 (51%) women stated that their spouses were against use of limiting and spacing methods, respectively; while 3 (0.8%) women reported contraception being a taboo in their household, others chose not to respond. Conversely, male sterilisation was considered acceptable by 46 (12%) women only; while 256 (66%) were against vasectomy, 88 (22%) were not aware of the method. The reasons attributed to non-acceptance of vasectomy, as reported by 80 participants, included their belief that sterilisation is women’s prerogative (39, 49%), fear of impotence and other side effects (21, 26%), stigma (8, 10%), religious beliefs (7, 8.8%) and non-popularity (5, 6.2%).
Contraceptive awareness and Ever-useAwareness of modern methods of contraception and reported ever-use in the study population is given in Figure 2. Among the 390 study participants, 247 (63%) women reported ever-use of modern contraception as a couple, with limiting and spacing methods adopted by 155 (40%) and 141 (36%) couples, respectively. Women cited their primary sources of contraceptive information as friends/relatives (55%), followed by healthcare providers (37%) and media (16%). Facility level healthcare providers, namely doctors and staff nurses contributed to contraceptive awareness in 242 (62%) and 124 (32%) women, respectively; while community level healthcare providers, namely female multipurpose health workers and Anganwadi workers, had provided information to 121(31%) participants.
Figure 2. Awareness and ever-use of contraceptive methods in the study population (n=390)
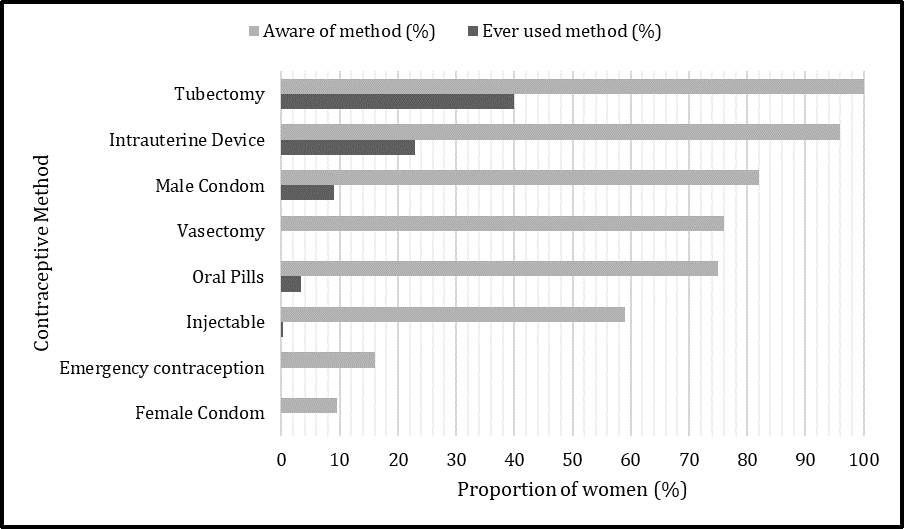
During interaction with a healthcare provider, 259 (66%) women reported being counselled at least once regarding modern contraceptive methods; spacing and limiting methods were offered to 196 (50%) and 182 (47%) women, respectively. Merely 139 (36%) women reported being offered a choice of more than one modern contraceptive method; 60 (16%) were offered three or more methods, while 79 (20%) were given two method choices. Female sterilisation and IUD were the most common provider-directed methods in 69 (18%) and 50 (13%) women, respectively; one (0.3%) woman was only offered combined oral pills.
Two hundred and twenty-two (57%) women reported recent use of female contraceptive methods in the preceding five years. Tubectomy (69.8%), IUD (28.4%), oral pills (1.4%) and injectable contraception (0.4%) was the method mix reported. Public health facilities were the service providers for 179 (81%) of them, with tertiary care facilities catering to 91 (41%) women; private facilities catered to 43 (19%) women. At the time of adoption of contraception, among the 222 recent users, 42 (19%) and 41 (19%) recalled being informed about the relative effectiveness of the method and symptoms or signs that necessitate a return to the health facility, respectively. Information regarding common side effects and mechanism of action of the method used were shared with 20 (9%) and 4(1.8%) participants, respectively. Among the 67 women who were currently using, or who had recently used modern spacing methods, 21 (31%) were counselled regarding return to fertility upon discontinuing use of the method. Moreover, of the 35 women who had approached healthcare providers for removal or switching of spacing methods, providers complied 83% of the time, while 6 (17%) women expressed dissatisfaction as their requests for removal or switching were not heeded.
Contraceptive coercionAmong the 222 recent contraceptive users, 181 women reported adopting the method voluntarily, which translates to 46.4% of the total study participants with a perceived need for contraception. The remaining 41 (10.5%) women reported contraceptive coercion by a healthcare provider in the immediate postpartum period; 33 (8.5%) and 8 (2.0%) women were forced or coerced, respectively. Tables 1 and 2 show the results of univariate analysis of contraceptive coercion with healthcare-related factors and socio-demographic determinants, respectively. A binomial logistic regression was performed with six predictor variables (Table 3), which was statistically significant, χ2(4) = 27.40, p < 0.001. The model explained 50.7% (Nagelkerke R2) of the variance in contraceptive coercion and correctly classified 87.8% of cases. Of the six predictor variables, three were found to be statistically significant: employment status, type of healthcare facility and method of contraception adopted.
Table 1. Association of contraceptive coercion with method and healthcare facility (n=222)
|
|
Number of contraceptive users, n |
Voluntarism in contraceptive use, n (%) |
P value |
||
|
Voluntary |
Coerced |
Forced |
|||
|
Type of Healthcare facility |
|
|
|
|
0.002* |
|
Public facility |
179 |
139 (78) |
8 (4.5) |
32 (18) |
|
|
Private facility |
43 |
42 (98) |
– |
1 (2.3) |
|
|
Level of healthcare facility* |
|
|
|
|
0.001* |
|
Primary care |
61 |
56 (92) |
1 (1.6) |
4 (6.6) |
|
|
Secondary care |
27 |
25 (93) |
1 (3.7) |
1 (3.7) |
|
|
Tertiary care |
91 |
58 (64) |
6 (6.6) |
27 (30) |
|
|
Method of contraception |
|
|
|
|
0.001* |
|
Tubectomy |
155 |
148 (95) |
1 (0.6) |
6 (3.9) |
|
|
LARC |
63 |
30 (48) |
6 (9.5) |
27 (43) |
|
|
SARC |
4 |
3 (75) |
1 (25) |
– |
|
|
Note. *Only public facilities are considered; LARC: Long-acting Reversible Contraceptives (includes IUD); SARC: Short-acting reversible contraceptives (includes Oral pills and Injectables). |
|||||
Table 2. Association of contraceptive coercion with socio-demographic determinants (n=222)
|
Sociodemographic variable |
Voluntarism in contraceptive use, n (%) |
P value |
|
|
Involuntary |
Voluntary |
||
|
Age in years |
|
|
0.081 |
|
19-24 |
13 (23) |
43 (77) |
|
|
25-30 |
26 (20) |
104 (80) |
|
|
> 30 |
2 (5.7) |
34 (94) |
|
|
Number of living children |
|
|
0.000* |
|
1 |
22 (50) |
22 (50) |
|
|
2 |
18 (12) |
139 (88) |
|
|
≥3 |
1 (5) |
20 (95) |
|
|
Education Status |
|
|
0.274 |
|
Illiterate |
1(33) |
2 (67) |
|
|
< 10 years of schooling |
13(24) |
42(76) |
|
|
≥ 10 years of schooling |
17(14) |
101(86) |
|
|
Graduate |
10(22) |
36(78) |
|
|
Employment status |
|
|
0.021* |
|
Employed |
1(3) |
29(97) |
|
|
Unemployed |
40(21) |
152(79) |
|
|
Religion |
|
|
0.953 |
|
Hindu |
33 (19) |
138 (81) |
|
|
Christian |
3 (14) |
19 (86) |
|
|
Muslim |
5 (18) |
23 (82) |
|
Table 3. Results from logistic regression model predicting likelihood of contraceptive coercion (n=222)
|
|
Adjusted Odds Ratio |
95% CI for Adjusted Odds Ratio |
P value |
|
|
Lower |
Upper |
|||
|
Age in years |
|
|
|
|
|
19 – 24 |
Reference |
|||
|
25 – 30 |
1.05 |
0.15 |
7.5 |
0.960 |
|
≥ 30 |
2.6 |
0.42 |
15.5 |
0.305 |
|
Number of living children |
|
|
|
|
|
1 |
Reference |
|||
|
2 |
0.81 |
0.064 |
10.2 |
0.868 |
|
≥ 3 |
1.06 |
0.11 |
10.0 |
0.956 |
|
Level of education |
|
|
|
|
|
0 – 9 years of schooling |
Reference |
|||
|
≥ 10 years of schooling |
1.3 |
0.36 |
4.5 |
0.707 |
|
Graduate |
0.43 |
0.13 |
1.4 |
0.150 |
|
Employment status |
|
|
|
|
|
Employed |
Reference |
|||
|
Unemployed |
13.1 |
1.3 |
127.6 |
0.027* |
|
Type of healthcare facility |
|
|
|
|
|
Private |
Reference |
|||
|
Public |
18.7 |
1.8 |
193.2 |
0.014* |
|
Method of contraception |
|
|
|
|
|
Permanent methods |
Reference |
|||
|
Reversible methods |
30.5 |
8.2 |
112.6 |
0.000* |
|
Note. CI: Confidence Interval |
||||
Discussion
Study participants reported a range of experiences of inadequate autonomy in relation to family planning decision making and access to contraceptive care. While at the household and community level, social norms and gender disparities operate to tilt the power balance in reproductive decisions towards the male spouse and other family members, the health system perpetuates this injustice by limiting access to essential contraceptive information, restricting the method mix offered, biasing contraceptive counselling to increase uptake, denying requests for method removal/switching, and coercing or non-consensual provision of provider-dependent methods.
Joint decision making with spouse was reported as the norm by more than half of the women when deciding on number or spacing of children; however, an increasing dominance of spouse and other family members was noted with respect to contraceptive decision making. Whether true consensus characterises these so-called “joint decisions” is doubtful, as women in this demographic are often overruled by their spouses [3]. Twenty-nine percent pregnancies in the preceding five years were found to be unintended. This contrasts favourably against the national estimate of 44% for India as reported by a global analysis of unintended pregnancy levels in the five-year period between 2015 and 2019[7]. While this may be due to Tamil Nadu having one of the highest contraceptive prevalence rates (65.5%) in India[10], the extent to which unreported abortions in this study may have contributed to the observed difference is not known. Three out of four unintended pregnancies were mistimed as opposed to unwanted; this finding concurs with the relatively low acceptability for reversible methods seen in this population.
While India has adopted the “cafeteria approach” for contraceptive service delivery, in which couples may choose from the available contraceptives depending on their needs, this was reportedly followed only in 36% of client-provider interactions in this study. Until recently, the basket of choice was limited in the national programme with only five modern contraceptives: three spacing methods (combined oral pills, male condoms, IUDs) and two limiting methods (tubectomy and vasectomy). Injectable contraceptives “Antara” and Centchroman pill “Chhaya” were added in 2015-16; while female condoms do not yet have a place in the contraceptive cafeteria, except as a targeted intervention for female sex workers in a few states. Other hormonal contraceptives such as progestin-only pills and subdermal implants are available only in the private sector. The method mix observed in this study indicates the programme has not, so far, succeeded in improving access to modern spacing methods. Neighbouring SEAR countries such as Bangladesh, Bhutan, Indonesia and Nepal offer at least seven contraceptives in the public sector, including implants[11, 12, 13]. National surveys from Sub-Saharan Africa indicate that gains in implant use have exceeded combined gains for IUDs, pills, and injectables[14]. Several studies indicate there is a positive correlation between number of contraceptive methods offered and willingness-to-use; the addition of every new contraceptive method, if made available to at least half of the population, increases the modern Contraceptive Prevalence Rate (mCPR) by 4–8%[2, 15].
The monopoly of IUDs among spacing methods offered in the public sector might be due to provider perceptions of better compliance as these methods require less periodic motivation compared to oral pills and condoms. However, evidence shows that women believe effectiveness is the most important criterion in choosing a contraceptive and that, when long-acting reversible contraceptives (LARCs) are available and affordable, 70-75% clients, if fully informed about method characteristics, will choose them of their own accord, with lower discontinuation and higher satisfaction rates[16]. Hence, the “WHO tiered-effectiveness counselling” approach in which highly effective methods are prioritised first, may be advocated for this purpose, after assessing appropriateness to our country context[17]. Limiting the contraceptive method mix and biased contraceptive counselling are subtle forms of coercion that may indirectly impact a woman’s reproductive autonomy[18].
Available evidence suggests that information given by providers to clients about contraceptive methods is frequently inadequate, as seen in the present study. As per the National Family Health Survey (NFHS)-4 data, only 47% of modern contraceptive users in India were informed about possible side effects. A smaller proportion of 39% were told about what to do if they experience side effects, while 54% were informed about other methods [19]. Qualitative data from southern India shows that providers were more likely to share information related to method effectiveness; while the less positive but relevant aspects such as side effects and contraindications are not discussed, so as not to deter potential acceptors[8]. A recent study in Mexico indicates that women regard complete and correct information as the most important aspect of an ideal contraceptive counselling [20]. Similarly, an Indian Council of Medical Research Task Force Study evaluated informed contraceptive choices among 8077 potential clients; it was seen that a majority of women opted for spacing methods and informed choice equipped the women to override provider bias in the selection of contraceptive method [21].
Contraceptive coercion was reported by a considerable number (10.5%) of study participants, with forced contraception or non-consented contraception, more frequently reported compared to the less overt, coerced contraception. This may be because, subtler provider biases and disregard for voluntary choice may not be perceived as coercion by clients, as shown by a study in Sub-Saharan Africa, where many women accepted the actions of providers as ultimately being in their best interest. Contraceptive coercion sits on a spectrum, rather than being a binary outcome; limiting free, full and informed choice in the absence of overt force or violence still constitutes coercion. While historically, coercion has been conceptualised as a unidirectional phenomenon, it can operate in both directions: upward coercion, which indicates “pressure to use when there is no desire to use” as compared to downward coercion, which is “pressure not to use when there is a desire to use”[18]. However, upward coercion is found to be more common across all identity groups[22].
Multivariate logistic regression showed that women reporting contraceptive coercion were more likely to have been unemployed (AOR: 13.1 [1.3,127.6], P=0.027) or to have sought intrapartum/postpartum care at a public health facility (AOR: 18.7 [1.8, 193.2], P=0.014). From one point of view, this could indicate the crucial role of financial independence in enabling a woman to be assertive in her reproductive choices and thereby, exercise her right to reproductive self-determination. On the other, the tacit support for coercive birth control practices and/or insistence on meeting population control targets by existing family planning programmes, may explain the strong association of this practice with public healthcare facilities. Its occurrence, predominantly in tertiary level public facilities (80%), calls for the strengthening of family planning services in primary and secondary level facilities, to share the load of the overburdened tertiary care facilities, which suffer from poor individual-centred care as a result. Emphasis on targets that give as much credit to promoting access to unbiased contraceptive counselling for women, irrespective of whether she accepts or declines contraception, may help deal with this form of structural coercion[18].
Female sterilisation and LARCs [4.8% (7/155) of the tubectomies and 52% (33/63) of the Postpartum Intrauterine Contraceptive Device (PPIUCD) insertions] were almost exclusively implicated in coercive practices. Reversible methods, (AOR: 30.5 [8.2, 112.6], P <0.001) in this case PPIUCD, had 30 times higher odds of being associated with contraceptive coercion. Studies conducted in India cite examples where women underwent sterilization or IUD insertion without their knowledge or explicit approval/consent, especially in urban public health facilities[8]. As contraceptive procedures are never an emergency, provision of inadequate time and information to clients to consent or obtaining third party consent to perform sterilisation cannot be condoned. According to the International Federation of Gynaecology and Obstetrics, “Only women themselves can give ethically valid consent to their own sterilization. Family members including husbands, legal guardians … cannot consent on any woman’s or girl’s behalf”[23].
Respect for autonomy is a crucial principle underlying most ethical frameworks addressing healthcare, with reproductive autonomy defined as “the power to decide about and control matters associated with contraceptive use, pregnancy, and childbearing” [24]. Client-Oriented, Provider-Efficient Services (COPE) is a quality improvement process built around the framework of seven clients’ rights and three staff needs. The underlying assumptions informing this process are that clients are not passive but active participants who are responsible for making their own decisions related to healthcare; and while healthcare staff desire to deliver high quality services, it will remain a challenge without adequate resources and infrastructure[25]. Evidence from Sub-Saharan Africa shows that while contraceptive coercion may have structural as well as interpersonal causes, much of the coercion reported stemmed from structural causes, and that contraceptive autonomy may be limited even by providers working in good faith[18]. While it is unacceptable for family planning services to be rendered with a utilitarian goal in mind; the potential ethical dilemmas arising during provision of care to women, who are ignorant of the dangers of too many and closely spaced pregnancies, deserves its mention.
This is one of the few studies in India to introspect on whether target-driven contraceptive services may contribute to women being pushed to adopt contraception they do not fully understand or want. Unlike most quality-of-care studies which are conducted as facility level exit surveys, the community-based nature of this study precludes courtesy bias to a great extent, as participants were able to respond freely without fear of offending their healthcare provider. However, our study has a few limitations. Study findings may be subject to recall bias, although this has been minimised by restricting the time horizon to the preceding five years. Experiences of adolescents and single, unmarried women, who face discrimination and a unique set of challenges in accessing contraceptive services could not be captured. Downward coercion is observed in this population, and this less-explored form of coercion needs further understanding.
Conclusion
At the outset, while essential contraceptive services are made accessible to the vast majority of women, the average contraceptive user is still far from equipped with the complete range of contraceptive information and services to allow for the full exercise of reproductive autonomy. Although positive gender dynamics is observed in the context of family planning, much remains to be done with regard to re-popularisation of vasectomy and improving acceptability and demand for modern spacing methods by promoting the “basket of choice” approach. It is the collective responsibility of healthcare professionals everywhere to implement a shared decision-making framework for contraceptive counselling; create safeguards and review mechanisms to protect the sanctity of informed consent; and show a strong commitment to ensuring that rights-based care in family planning becomes a reality.
Authors: Shruthee SG (corresponding author — [email protected], https://orcid.org/0000-0001-7843-9329), Department of Community Medicine, Government Stanley Medical College, and Technical Officer, Resource Group for Education and Advocacy for Community Health (REACH), Chennai, Tamil Nadu, INDIA; Senthil Arasi ([email protected], https://orcid.org/0000-0003-2060-375X), Assistant Professor; Seenivasan P ([email protected]), Professor and Head, Department of Community Medicine, Government Stanley Medical College, Chennai, Tamil Nadu, INDIA.
Conflict of Interest: None to declare. Funding: None.
Acknowledgements: The authors are immensely grateful to Dr TK Sundari Ravindran, and Dr Subha Sri Balakrishnan, whose comments were invaluable to the revision and content validation of the study measures.
Ethics approval: Approval was obtained from the Institutional Ethics Committee of the government-run Stanley Medical College, Chennai.
Statement of similar work: The present study was conducted to fulfil part of an MD dissertation entitled “Person Centred Care in Family Planning among Women in Kanchipuram, India – A community based cross-sectional study”
Data sharing: Data not made available in public domain. Please contact corresponding author for access to raw data.
To cite: Shruthee SG, Arasi S, Seenivasan P. Voluntary and rights-based family planning for women: Observations from a community-based study in southern India. Indian J Med Ethics. 2025 Jul-Sep; 10(3) NS: 183-190. DOI: 10.20529/IJME.2025.010
Submission received: September 30, 2023
Submission accepted: August 13, 2024
Published online first: February 12, 2025
Manuscript Editor: Sunita Sheel Bandewar
Peer Reviewer: Shaibya Saldanha
Copyright and license
©Indian Journal of Medical Ethics 2025: Open Access and Distributed under the Creative Commons license (CC BY-NC-ND 4.0), which permits only noncommercial and non-modified sharing in any medium, provided the original author(s) and source are credited.
References
- Santhya KG. Changing family planning scenario in India. South & East Asia Regional Working Paper no. 17. New Delhi: Population Council; 2003 [cited 2025 Jan 13]. Available from: https://knowledgecommons.popcouncil.org/cgi/viewcontent.cgi?article=1526&context=departments_sbsr-rh
- Muttreja P, Singh S. Family planning in India: The way forward. Indian J Med Res 2018 Dec;148(Suppl 1):S1. https://doi.org/10.4103/ijmr.IJMR_2067_17
- United Nations Population Fund (UNFPA) and Hera. Research on what determines women’s ability to decide on their SRHR and the relationship between this and other aspects of their lives. Volumes 1 and 2: Final report. New York. 2019[Cited 2023 Sep 13]. Available from: https://www.unfpa.org/sites/default/files/resource-pdf/UNFPA_HERA_5-6-1_CLEAN_02_March1.pdf
- FP2030: Commitments. The Comprehensive Human Rights-based, Voluntary Family Planning Program Framework. [cited 2025 Jan 13]. Available from: https://www.fp2030.org/resources/the-comprehensive-human-rights-based-voluntary-family-planning-program-framework
- United Nations. SDG Progress Report. Goal 5: Gender Equality. 2023[cited 2024 Apr 16]. Available from: https://unstats.un.org/sdgs/report/2023/Goal-05/
- Asian-Pacific Resource & Research Centre for Women (ARROW). An advocate’s guide: integrating human rights in universal access to contraception. Malaysia. 2016[cited 2023 Sep 15]. Available from: http://arrow.org.my/wp-content/uploads/2017/02/AdvocateGuide_2016_webready.pdf
- Guttmacher Institute. Unintended Pregnancy and Abortion Worldwide. New York. 2022 [cited 2023 Sep 18]. Available from: https://www.guttmacher.org/fact-sheet/induced-abortion-worldwide
- Koenig MA, Foo GH, Joshi K. Quality of care within the Indian family welfare program: a review of recent evidence. Stud Fam Plann 2000 Mar;31(1):1-8. https://doi.org/10.1111/j.1728-4465.2000.00001.x
- Shruthee SG. A Community Based Cross Sectional study on Person Centred Care in Family Planning among Women in Kancheepuram District, Tamil Nadu. MD thesis. The Tamil Nadu Dr. MGR Medical University. Chennai, India. 2020[cited 2023 Sep 13]. Available from: https://www.tnmgrmu.ac.in/index.php/library.html
- International Institute for Population Sciences (IIPS) and ICF. National Family Health Survey (NFHS-5), India, 2019-21: India and 14 States and UTs (Phase II). Mumbai. 2021 [cited 2023 Sep 13]. Available from: https://mohfw.gov.in/sites/default/files/NFHS-5_Phase-II_0.pdf
- Press Information Bureau. Usage of Modern Contraceptives. India. 2020 [cited 2023 Sep 25]. Available from: https://pib.gov.in/newsite/PrintRelease.aspx?relid=200315
- United States Agency for International Development. Modern Methods of Contraception in India: The Potential of Progestin-only-pills and Centchroman. Washington DC. 2016 [cited 2023 Sep 24]. Available from: https://pdf.usaid.gov/pdf_docs/PA00W86D.pdf
- Weerasinghe M, Agawane S, Karandikar N, Fisher J, Sastry J. Examining the place of the female condom in India’s family planning program a qualitative investigation of the attitudes, opinions of key stakeholders in Pune, India. BMC Public Health 2022 Dec;22(1):1-1. https://doi.org/10.21203/rs.3.rs-1029166/v1
- Jacobstein R. Liftoff: The Blossoming of Contraceptive Implant Use in Africa. Glob Health Sci Pract 2018;6:17–39.https://doi.org/10.9745/GHSP-D-17-00396
- Pariani S, Heer DM, Arsdol MDV. Does Choice Make a Difference to Contraceptive Use? Evidence from East Java. Stud Fam Plann 1991; 22: 384. https://doi.org/10.2307/1966452
- World Health Organization. Beyond Acceptability: Users’ Perspectives on Contraception. Reproductive Health Matters. [cited 2023 Sep 25]. Available from: https://iris.who.int/bitstream/handle/10665/42012/0953121003.pdf?sequence=1&isAllowed=y
- Stanback J, Steiner M, Dorflinger L, Solo J, Cates W. WHO Tiered-Effectiveness Counselling Is Rights-Based Family Planning. Glob Health Sci Pract 2015; 3: 352–7. https://doi.org/10.9745/GHSP-D-15-00096
- Senderowicz L. “I was obligated to accept”: a qualitative exploration of contraceptive coercion. Social Science & Medicine 2019; 239: 112531. https://doi.org/10.1016/j.socscimed.209.112531
- International Institute for Population Sciences (IIPS) and ICF. National Family Health Survey (NFHS-4), 2015-16: India. Mumbai. 2017[cited 2023 Sep 13]. Available from: https://dhsprogram.com/pubs/pdf/fr339/fr339.pdf
- Holt K, Zavala I, Quintero X, Mendoza D, McCormick MC, Dehlendorf C, et al. Women’s preferences for contraceptive counselling in Mexico: Results from a focus group study. Reproductive Health 2018;15:128. https://doi.org/10.1186/s12978-018-0569-5
- Baveja R, Buckshee K, Das K, Das SK, Hazra MN, Gopalan S, et al. Evaluating contraceptive choice through the method-mix approach. An Indian Council of Medical Research (ICMR) task force study. Contraception 2000; 61:113–9. https://doi.org/10.1016/s0010-7824(00)00089-5
- Swan LE, Cannon LM, Lands M, Higgins JA, Green TL. Coercion in contraceptive care: differences based on racial/ethnic identity, sexual orientation, and gender identity. Contraception 2023 Nov 1;127:110232. https://doi.org/10.1016/j.contraception.2023.110232
- International Federation of Gynaecology and Obstetrics. Guidelines: “Female Contraceptive Sterilization”. (para. 7,8) June 2011[cited 2023 Sep 25]. Available from: http://www.wunrn.org/news/2011/06_11/06_27/062711_female.htm
- Upadhyay UD, Dworkin SL, Weitz TA, Foster DG. Development and validation of a reproductive autonomy scale. Stud Fam Plann 2014 Mar;45(1):19-41. https://doi.org/10.1111/j.1728-4465.2014.00374.x
- Engender Health. COPE for reproductive health services: a tool book to accompany the COPE handbook. New York, NY: Engender Health; 2003[cited 2025 Jan 13]. Available from: https://www.globalhealthlearning.org/sites/default/files/page-files/COPE Handbook -A_Process_for_Improving_Quality_in_Health_Services.pdf
