ARTICLE
A critical ethnography of doctor–patient interaction in southern Iran
Ahmad Kalateh Sadati, Mohammad Taghi Iman, Kamran Bagheri Lankarani, Soghra Derakhshan
DOI: https://doi.org/10.20529/IJME.2016.042
Published online: April 16, 2016
Abstract
Doctor–patient interaction is a subject with ethical ramifications, besides being an important issue in medical sociology. The main goal of this critical study is to explore the interactional experience of hospital admitted patients. For this reason, the study, carried out in an educational hospital in southern Iran, entailed 156 recorded clinical consultations, 920 hours of participant observation, and six focus groups consisting of patients and their families. The research method used is Critical Ethnography, which was introduced by PF Carspecken. The results showed that negative interactional experience was common among the participants. Six related themes were: doctors’ inattentiveness; weak interaction; violation of patients’ privacy; unjustified pain; long waiting period and ambiguity; and faceless physicians. According to the participants’ observations, poor interaction with doctors has led to these negative experiences. The findings showed that doctors were inconsiderate about patients’ concerns and due to this, patients were dissatisfied. Theoretically, this form of fragmented collaboration has deep roots in the framework of modern medicine, but in the context of this study, the intensity of the fragmentation between doctors and patients was observed to be intolerable. To solve this problem, models of patient-centredness and narrative medicine are recommended. In addition, the health system should monitor and evaluate the observance of ethics by physicians.
Introduction
Doctor–patient communication is an important issue in the field of medicine (1, 2, 3, 4, 5). It is an interpersonal process and essential to relationship-centred care (3). The interaction needs to be tangible. Evidence-based research shows that effective doctor–patient communication is related to outcomes such as enhanced patient satisfaction, better treatment compliance and better symptom solution. Since, medical intervention is a process that aims to help patients (6), for success in this, the doctor should ensure active interaction.
This major subject of discussion since the time of Hippocrates became the focal point of debate in the medical and social sciences in the late 20th century (1, 7, 8). There have been several changes in the definition of the doctor–patient interaction in the western societies since the 1960s (9). Parsons, a prominent sociologist, introduced the term “sick role” in his textbook, The Social System. This term signifies that the patient has two rights and two obligations when consulting the doctor. The patients’ rights are that they are exempted from normal social roles and responsibilities, while their two obligations are to try to get well and to cooperate with medical professionals (10). The sick role theory has an important role in functionalist outcomes such as doctor–patient satisfaction, the efficacy of the interaction, productivity, responsibility and trust. Despite it being a successful theory, some believe that it legitimises asymmetrical relations between doctors and patients (11, 12).
The doctor–patient interaction has also been represented as a relationship characterised by dominance or coercion (9), which is parallel to the Parsonian theory. Simultaneously, another sociological theory, known as the critical theory, has been introduced by M Foucault and J Habermas and is being debated (7, 8, 12). Foucault sees modern medicine as a knowledge–power discourse (12, 13, 14, 15). Habermas views the power of medical experts and institutions as leading to a relationship that dominates over a patient’s life world, due to their instrumental rationality (16, 17, 18). These theories are the foundation for many researchers to explore the subject of the doctor–patient relationship (1, 19, 20, 21).
This study was conducted on the premise that a good doctor– patient interaction has positive effects on the patient’s health and satisfaction. This topic can be evaluated from several theoretical viewpoints. The main objective of this study was to evaluate patients’ opinions of their doctors’ interaction in the light of the critical theory. Our specific objectives were: (i) to explore the interactional lived experiences of patients and their families with doctors; (ii) to identify different aspects of interactional lived experiences; (iii) to extract the validity claims related to those aspects (horizon analysis); and (iv) to explore the theoretical analysis of the organisational mechanisms for doctor–patient interactions. Based on critical realism ontology that objective findings need to be explored, we have theoretically explained the reality of the doctor–patient interaction exploring real mechanisms. Therefore, our findings will be analysed discovering real mechanisms which make up this type of doctor–patient interaction.
Materials and methods
This qualitative study based on the critical paradigm was conducted in Shahid Faghihi Hospital, Shiraz, Iran, from January to August 2014. Data were collected using the following three methods:
- A total of 156 clinical consultations were audio recorded for 8 hours 28 minutes. Eight specialists cooperated with us—four cardiologists, three internists, and a neurologist. After getting verbal consent from patients, the sessions were recorded, transcribed and analysed.
- Participant observations were done for 920 hours in all hospital wards. Participant observation is defined as a “research that involves the social interaction between the researcher and informant in the milieu of the latter, during which data are systematically and unobtrusively collected” (22). According to Gold, there are several forms of participant observations, which include: the complete participant; the participant as observer stance; the observer as participant stance; and the complete observer (23). In this study, we used the first form, ie, the complete participant. The researcher as a clinical supervisor was a member of the group and his role was not revealed. Since qualitative research has idiographic features and is dependent on the context during participant observations, Epoche was used as the main instrument for validity (24). This was done to eliminate all biases about the hospital and doctor–patient interaction. Data collection and analysis were carried out in a theoretical manner without any prior knowledge or bias about the subjects. Also, due to the importance of reflexivity and the iterative nature of qualitative research, data collection and analysis were done by the reflexive method. Thus, the researcher presented the data and results to experienced clinicians (as thesis advisor) as well as to a thesis supervisor to minimise biases.
- Interviews with patients and their families were done in six focus group discussions (FGDs), in five wards of the hospital. Since patients in some wards such as the CCU and cardio surgery were in a critical condition, the FGD was done with patients who had passed their critical period and were in the out-of-bed (OOB) state and able to participate in FGDs. After getting their consent, the interviews were recorded and then transcribed. The focus groups information is given in Table 1. The interview questions were: (i) What is your opinion about the relation and interaction of your doctor with you in this hospital? (ii) How do you evaluate this interaction? and (iii) What were your expectations from the physicians?
| Table 1: The information from focus group discussions (FGDs) | |||||||
| S.No. | Ward | Number of participants | Female | Male | Patients number | Patient families | Duration of interview (hour) |
| 1 | Internal | 6 | 2 | 4 | 5 | 1 | 1:10 |
| 2 | Urology | 11 | 5 | 6 | 5 | 6 | 1:28 |
| 3 | CCU | 16 | 7 | 9 | 13 | 3 | 1:15 |
| 4 | General surgery No. 1 | 5 | 5 | 0 | 4 | 1 | 1:20 |
| 5 | Cardio surgery | 5 | 3 | 2 | 0 | 5 | 1:12 |
| 6 | General surgery No. 2 | 8 | 1 | 7 | 7 | 1 | 0:42 |
| Total | 51 | 23 | 28 | 34 | 17 | 7:07 | |
Data were analysed by a critical method which focuses on the power relations in social interactions. For the issue of doctor–patient interaction, the critical approach evaluates the asymmetrical power relations between a doctor and a patient. In this study, Carspecken’s critical ethnography was used for data analysis (25, 26). Though this method was first used in the field of education (25, 26, 27), many healthcare researchers have applied it in the past decade (28, 29, 30). Carspecken’s method of reconstructive analysis focuses on one category of action, ie cultural milieu or the norms, values and beliefs of the people who are being studied. In this analysis, utterances are analysed according to three main claims which are called subjective, objective, normative/evaluative. Subjective claims are about the existing subjective states of mind; objective claims assert that certain objects and events exist, and normative/evaluative claims that others should agree to the fitness, goodness and appropriateness of certain activities (25). In this method, data analysis is completed with observer comments (OC) that are related to researchers’ participant observations and interpretation of clinical interactions.
This study was based on the ethical codes of the American Sociological Association (31) and 7th revision of the Declaration of Helsinki on research ethics (32). Based on these considerations and the ethics of research, names of all physicians and patients in this study are fictional. The privacy of patients was also taken into consideration.
Results
Participant observations showed that some patients were ignored by physicians, especially in the surgical wards, which led to negative experiences for patients. Although patients were visited by residents or interns on a daily basis, this did not satisfy the patients. The interactional experience of patients and their families with physicians revealed that during their stay at the hospital, they had experienced several negative interactions due to weak and passive relationships with doctors. The utterances regarding negative interactional experiences of patients’ and their families, in six extracted categories, are as follows:
Doctor’s inattentiveness
One theme related to negative interactional experiences is the experiences of being neglected by the physician. Generally, this is due to doctors’ disregard for patients’ needs and concerns. It means that the physician does not visit the patient regularly, in some cases only once in three/four days or once a week. The experience of doctor’s inattentiveness involves specific features, which suggest that the patient does not have any clear understanding about his/her illness and the treatment process.
OC [observer comments]: Due to the training and educational system of healthcare in this hospital, there was a huge interactional gap between physicians and patients. In this setting, a physician is a scientific faculty member (SFM) and a patient is assigned under his supervision, who has other obligations such as: teaching medical students, interns, residents, and sometimes fellowship physicians. Due to the structure of the teaching system, SFMs do not have a direct connection with patients and many medical students practise their role in a hierarchical order. Though patients and their families have trust in medical students, they expect to be visited by SFMs even for a few minutes in order to get an explanation about the process of their treatment. Participant observations showed that the inattentiveness of SFMs in the surgical wards was more tangible than in internal and cardiology wards. Patients and their families insist that although medical students visited them often, they felt that SFMs’ visit is more important. Another aspect is related to a doctor’s personality. Evidence showed that patients who complained about this issue were afraid to discuss it with their SFMs and medical students. Besides the problem of hierarchy, doctors ignore their patients because of poor structure of the health system.
Meaning unit 1; I was in the emergency ward; they asked me who my doctor was; and I answered, “Dr Sa’idi”, but I haven’t seen her in the past month; how can a patient be aware of his/her illness or treatment? What if the patient is not satisfied with the treatment, Well, I’m not aware of the quality of my [father’s] treatment [patient’s son with a surgical problem].
Meaning unit 2: I was admitted here four days ago, but I don’t know who my physician is, if anyone comes and says that I’m Dr Ma’roof, I’d easily accept it [woman with urology problem].
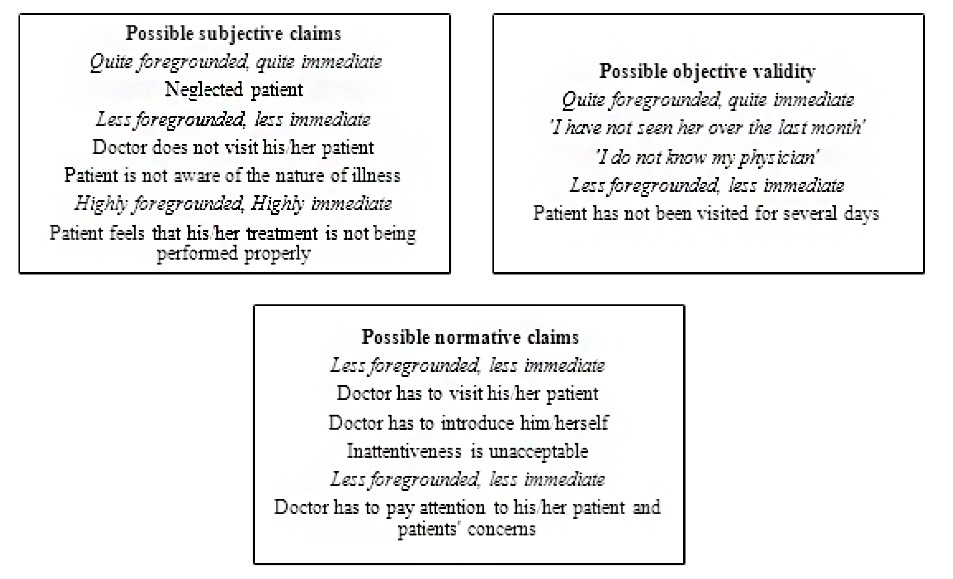
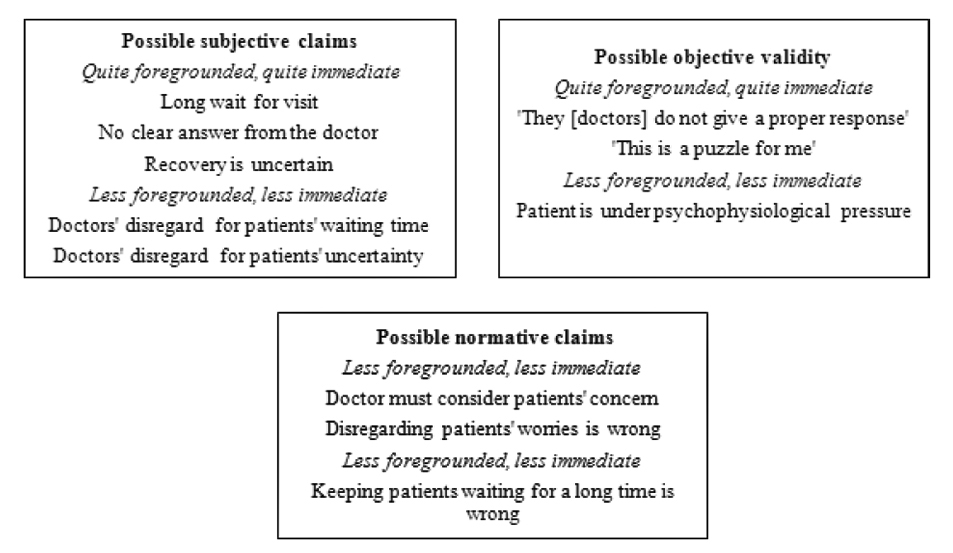
As these meaning units show the experience of being neglected by physicians is associated with physicians’ disregard for patients by not visiting them. The horizon analysis of doctors’ inattentiveness is shown in Figure 1.
In Figure 1, interactional experiences specifically show that patients felt that they were ignored by physicians and felt dissatisfied. A forgotten patient can be described as one who thinks his/her admission is ineffective. Common utterances regarding the doctor’s inattentiveness are: “I have not seen the doctor”, “I do not know my doctor”, and “I have not been visited by the doctor”. In this situation, patients and their families become angry and feel dejected, but they conceal their feelings because of asymmetrical power relations. In this scenario, they are unlikely to make a complaint to the supervisor in-charge or the hospital manager.
Weak interaction
Weak interaction refers to poor communication skills of doctors. It means that the doctor is unable to establish a proper relationship with the patient. Proper relationship means: to be a good listener, good explainer, and have good eye contact with the patient. A sign of weak interaction was that the physicians saw 156 patients in 8.28 hours, ie each consultation lasting on an average about 3 minutes. Considering the fact that these were specialist consultations such as cardiology, neurology and internal medicine, these sessions seem too short. An important reason is that physicians neither speak nor do they listen, and the non-verbal interaction is a rarity.
OC: Generally, daily visits included reports given by the residents or other medical students to SFMs. Overall, SFMs do not ask any question or give any explanation to patients. However, if a patient has a question he/she might answer the question or most likely refer the patient to his/her students. Still, this does not necessarily mean that medical student’s interact better with patients. A majority of them mimic their teacher’s interaction. For example, if a patient is suffering from pain, the standard practice is to inject lenitive without interaction or examination. All verbal and nonverbal interactions are weak.
Meaning unit 1: There is no proper question and answer session between the patient and the doctor. So far, we did not see this in this hospital. There is no conversation or interaction between the doctor and the patient at all (Woman’s husband).
Meaning unit 2: When the doctor arrives, he quickly takes a look at the patients. We are frustrated; we expect the doctor to talk to us. The doctor arrives for a few minutes, smiles and then leaves. It is so quick that it feels like a photo opportunity with the doctor (Patient’s son).
Meaning unit 3: There is a doctor who has visited our neighboring patient in the past three days, but he does not introduce himself and does not interact with the patient. He arrives, reads the reports, and gives some orders and leaves. Maybe the patient wants to talk with the doctor about his pain (Patient’s sister).
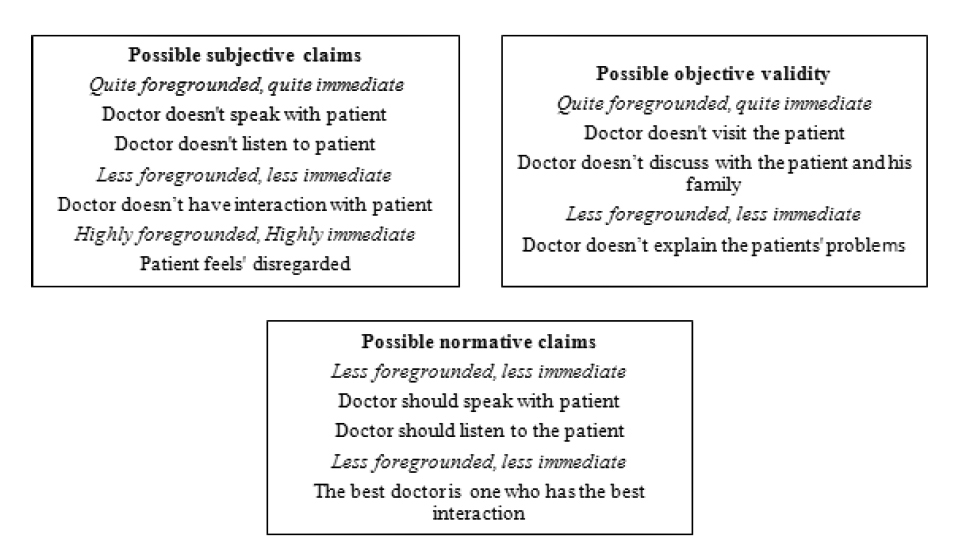
According to the horizon analysis, doctors did not have good interaction. A good interaction means to have a good discussion, listen and have non-verbal interaction. Where interaction is poor, patients and their families feel that they did not receive an effective consultation. (Figure 2)
Violation of patients’ privacy
Patient privacy is a right; every patient expects his/her physician to consider this issue very seriously. In the context of our study, this issue is noteworthy due to cultural and traditional values, especially for women.
OC: Participant observations showed that patients’ privacy is not considered as an important issue by physicians as well. This is a problem concerning physical examination, especially during surgical procedures. Observation showed that physicians disregard concerns involving patients’ privacy. For example, change of dressing of such body parts as the breasts, legs, or thighs was done with minimum concern for privacy. It seems that this is due to physicians’ disregard for patients’ sensitivities to such issues.
OC: Simin is a 37-year-old woman with a urinary problem. She was examined under the cystoscopy procedure 2 hours ago by two male residents and one male SFM from the urology department. Her expectation was to be examined only by the SFM without the presence of male residents.
Related meaning units: I trusted my physician; I wanted to be examined only by my physician, but I was examined in the presence of three male physicians; this is not right! After this I will never trust any physician. I am a woman; how can I trust physicians?
[OC]; Simin continued to cry, and her face was flushed.
OC: Zari is a 52-year-old woman who was diagnosed with breast cancer. Today, she had a mastectomy. In the operation room her breasts were examined by five or six medical students in the presence of the SFM. She had a terrible experience and she felt that her privacy was violated. She was very angry and said that except for her SFM she won’t allow students to perform any other procedure.
Related meaning units: I went to the operation room; five or six students examined my breasts. Do you think this is ok? I’m a woman; from now on, I will allow only my SFM to change my dressing and I won’t allow anyone else to touch me at all. Do you think it is right that a woman be examined by several male physicians?
[OC]: Zari was so angry about this issue that she did not complain about the surgical pain.
As these meaning units show, these two women had a bad experience and thought that their privacy was violated. Zari’s experienced emotional crisis included distrust in the medical institution and physician’s behaviour, specifically violation of privacy. Even though her operation was extremely painful, she felt that violation of her privacy was more important than the pain she was enduring. It could result not only in emotional crisis and mistrust, it could also result in silencing patients about emerging symptoms. Horizon analyses of unit meanings are shown in Figure 3.
As validity claims show, patients had a bad experience with doctors’ violating their privacy, which led to patients’ mistrust. In this study, trust is a gender-dependent issue and doctors’ disregard for the female body is the main reason for the negative lived experience. Simin and Zari were both emotionally and psychologically distressed. According to our finding, patient privacy is more important for women than men and if a physician ignores it, it can lead to emotional crisis and patient mistrust.
Unjustified pain
Unjustified pain alludes to insufficient treatment or inadequate consideration by physicians. This theme showed that physicians are not sensitive towards patients’ pain because theylack empathy. Also, this could be due to insufficient training in pain management or they may have the knowledge but they do not put it into practice.
OC: Observations showed that some procedures were performed without any consideration for the severity of pain. Physicians, such as surgeons or radiologists, performed their procedures without any prescription drug to reduce the pain. The general approach in these procedures is to inject lidocaine at the site of operation. Due to the asymmetrical power relation, the patient did not reveal his/her pain and tried to tolerate it as much as possible. Only rarely, if a patient complained more than usual, the physician would prescribe a narcotic.
OC: Complaint from an Iraqi woman’s husband. His wife had metastatic cancer and had to undergo a nephrectomy tube insertion. The previous day, a right nephrectomy tube was inserted into her right kidney without considering the level of pain. Today, there was a plan for a nephrectomy insertion into her left kidney, but her husband objected to performing the same procedure under similar conditions. This was because of his wife’s unjustified pain that she had experienced during the course of the previous tube insertion. He tried to convince the medical team to prescribe a narcotic; but his request was denied.
Related meaning units (Patient’s husband): She needs morphine. It [pointing to the size of the nephrectomy tube] is too long to be inserted into her body! She has pain, she needs morphine.
OC: Zahra, a 35-year-old woman with renal stone, who was operated yesterday.
Related meaning units: I was operated yesterday; my operation went off well, but after the operation, the doctor did not visit me at all. As I have had pain, I have been yelling since yesterday; the doctor should have visited me.
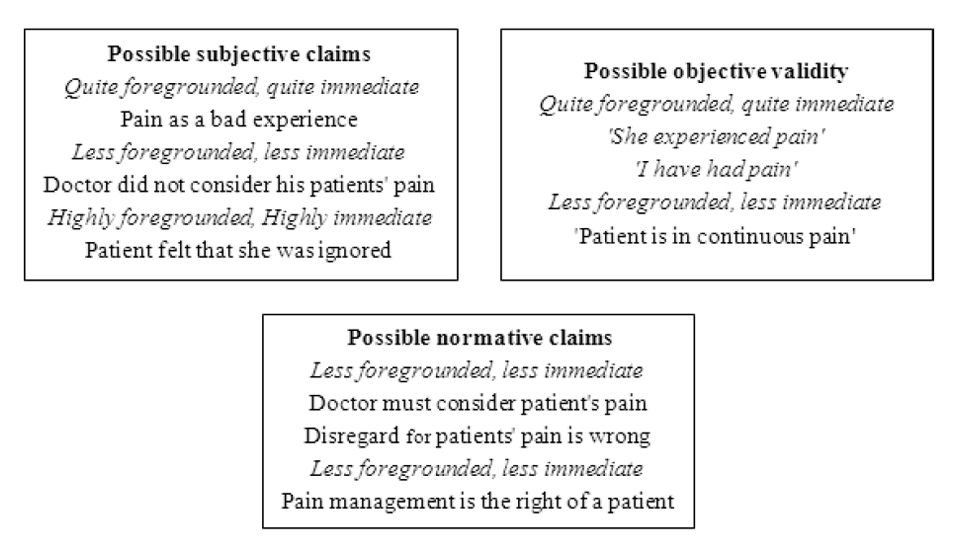
The horizon analysis of these meaning units is shown in Figure 4.
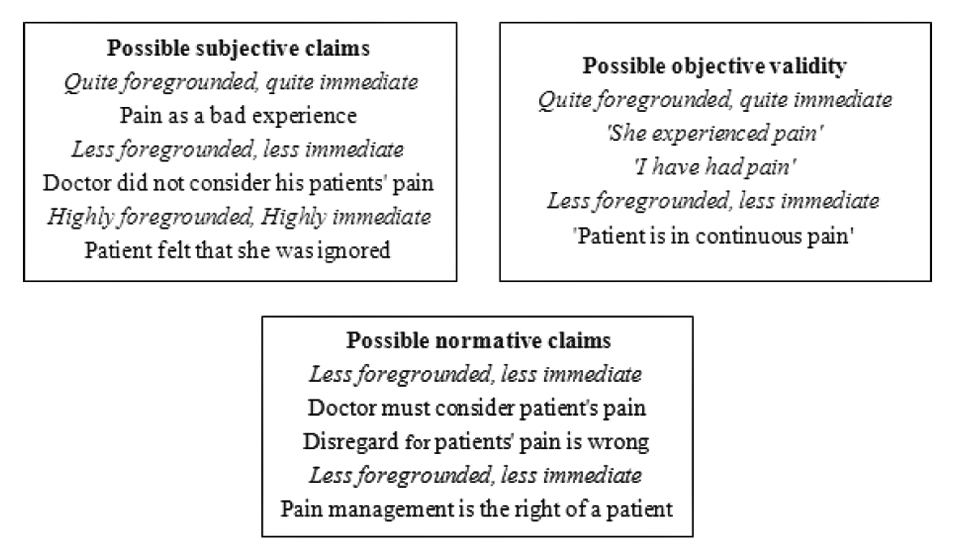
The two meaning units are about toleration of unjustified pain. According to validity claims, pain is a bad experience and normative/evaluative claims assert that subsiding pain is a patients’ right that should be respected by the physician.
Long waiting period and ambiguity
Patients and their family need to be informed about their disease, treatment and recovery period. When a doctor disregards these concerns, the patient is confronted with many unanswered questions and ambiguities. At the same time, something that makes this scenario even worse is the long waiting periods that they have to face to be visited by the SFMs or in some cases not being visited at all. Thus, the patient does not have a clear understanding of his/her condition.
OC: Observations showed that in surgical wards, some patients are unhappy, because they are not visited by their physicians. This leads to uncertainty about their illnesses and treatments. Although there seems to be no correlation between visits and recovery, especially in the case of complex illnesses, doctors’ explanation can help the patient in reducing their anxiety. Patients think that if a doctor visits them their illness will be cured. Although this assumption is seemingly false, it can reduce the ambiguity that leads to patients’ discomfort.
OC: The father of a patient who was admitted to the open heart surgery ward with Tetralogy of Fallot (TOF): His daughter did not have a successful recovery and was hospitalised for 3 months. He believed that her doctors did not give him a clear answer and his family was confused.
Related meaning units (Patient’s father): They [nurses] said that the doctor is coming soon, it was 9 o’clock, then 10, and now it is 11, yet he has not showed up. It seems that he will not come today either. I want to know what is happening to my child. I want to know why all of this has happened in the first place, they [doctors] don’t give a proper answer.
OC: Tahereh a woman with recurrent metastatic cancer. Related meaning units: When we ask about our illness, they don’t give a clear answer; for example, I asked the doctor about what are his plans for me? But he only said that I should be patient for the next fifteen months for doctor’s decision about my illness, and then he would think of something! This is puzzling me, what should I do?
Figure 5 shows the horizon analysis of this theme.
According to the findings, patients are confronted with an unclear understanding of their treatment plan, due to poor interaction.
Faceless physicians
An interaction occurs when there is collaboration. A good doctor–patient interaction happens when a patient is familiar with his/her physician. When a physician introduces him/herself to the patient, it leads to patient satisfaction. A faceless physician refers to a kind of doctor–patient interaction where the patient does not know his/her physician; in addition, he/she has never seen the physician. The patient only knows that he/she has been admitted for a specific physician’s service; he has heard the name of the physician and nothing more.
OC: Participant observations show that doctors seldom introduce themselves to their patients. In the present structure of the educational system, a medical team includes students, interns, residents, and SFMs who visit patients. In this scenario, none of the team members introduce themselves and, in some cases, SFMs do not even bother to make their rounds; they shift their responsibilities onto medical students. Under such circumstances, there is no connection that can lead to the patient’s familiarity with the physician
OC: Mehri is a woman with coronary vascular disease of focus group no. 3.
Meaning units related: No one introduces him/herself to the patient, not even the doctor. Since the time I was admitted to the hospital, I haven’t seen my doctor.
OC: Shadi, with renal stone disease, of participant observation.
Meaning units related: This was the first time that I was operated on by Dr Fariman. But I still do not know who he is, when I was taken to the operation room, I did not know which one of them was my doctor. Then I was carried to the operation room from the emergency room. Even if he visits me now I cannot recognise him.
Figure 6 shows the horizon analysis of this theme.
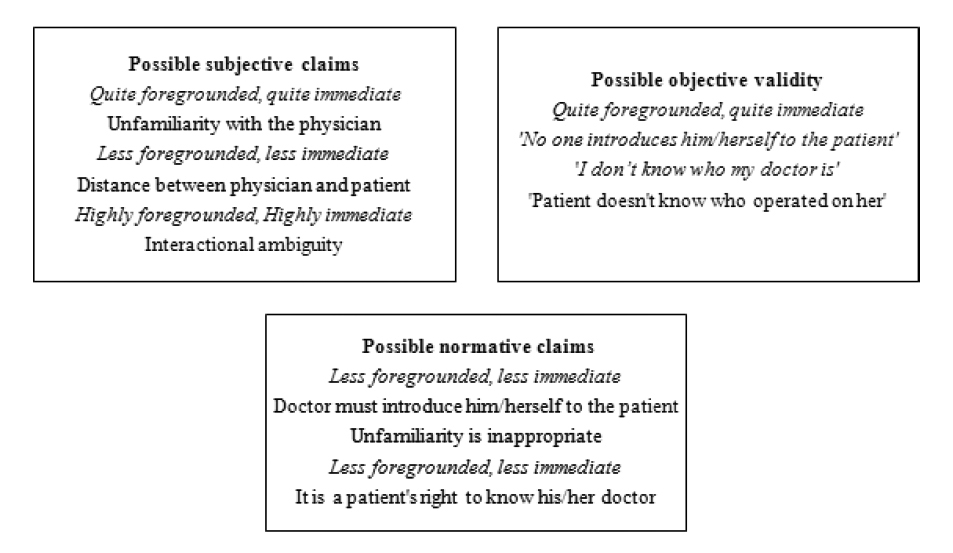
As shown in Figure 6, a poor interaction leads to patients’ unfamiliarity with their doctors. Under such circumstances, generally SFMs do not introduce themselves and they rarely visit their patient. In this condition, the patient is confronted with a faceless doctor.
Discussion and exploring real mechanisms
The results of this study showed that a poor interaction leads to doctors’ inattentiveness; violation of patients’ privacy; weak interaction; unjustified pain; long waiting period and ambiguity, and faceless physician. These negative experiences have led to patients’ unusual dissatisfaction, which was shown in participant observations and statements of FGDs. Due to the asymmetrical power relationship and domination of physicians’ power, neither patients nor their families express their dissatisfaction or concerns to the physicians. Our findings confirm the work of other scholars (1, 7, 8, 19, 21).
Cordella points out that even though patients seek help from, and mostly align with, medical authority, they do not like doctors who display a sense of superiority (1). Sadati and his colleagues showed that asymmetrical power relations lead to suppression of patients in consultations (7, 8). Atkinson’s research showed that medicine has several voices, some of which are inevitably unrelated to medical procedures (33). Although this claim is acceptable, what is important is that patients are dominated by the physicians, regardless of the type of voices.
On the other hand, Barry et al showed that the nature of an interaction depends on the type of voice used by doctors and patients. It is also related to the nature of the illness. For example, the worst outcomes occurred where patients used the voice of the lifeworld but were ignored (lifeworld ignored) or blocked (lifeworld blocked) by doctors’ use of voice of medicine (chronic physical complaints) (21).
Our study shows that the doctor–patient interaction is dominated by the physicians’ power rather than the nature of interaction. When doctors do not visit patients and this neglect becomes a normal behaviour for them, it can be asserted that the doctor–patient interaction is so asymmetrical that the physician interacts any way that he/she decides.
One of the aims of this study was to conceptually evaluate the reality of infrastructure mechanisms of doctor–patient interactions. For this reason, the discussion is done at a theoretical level. Thus, part of this debate is conceptual and is not related to our studied data. Hence, our discussion will answer this fundamental question: “Why is doctor–patient interaction poor?”
In superstructure analysis, the main reason for this kind of interaction seems to be the association of the educational system with healthcare. The hierarchical system of care on the one hand, and combining education and treatment on the other, creates a gap between SFMs and their patients. However, discussions about infrastructure mechanisms show us another aspect of poor doctor–patient interaction.
Habermas defined modern medicine as a system of experts (17, 18). This system dominates patients’ lifeworld and is ignored by physicians. Mishler, a pioneer researcher, showed that there is a conflict between medicine as a system and the patients’ lifeworld. So “the voice of lifeworld” is dominated by the “voice of medicine” (19). In this respect, modern medicine is evaluated as a one-dimensional system in which lifeworld is completely ignored (7). According to Edwards, modern medicine as a system consists of a body of expert, medical knowledge shaped by science and technology which is in contrast to health and is a part of the “system” rather than the “lifeworld” (34). On the other hand, according to Foucault, modern medicine is an unequal knowledge–power relationship (7, 13). Thus, modern medicine is an asymmetrical system based on experts’ power that includes a linear and instrumental model of diagnosis and treatment, which is the cause of suppression of patients.
According to this theoretical viewpoint, what happened in our study is a shape of ignorance and the suppression of lifeworld by the system. Critical theories and the results of our study suggest that our doctors are in such a superior position that they suppress the patients’ lifeworld, which leads to patients having little or no trust in doctors. This means that although patients may be satisfied with their treatment, they are disappointed with the interaction with their doctor. Thus, the doctor–patient interaction is in a fragmented state. FGDs explain this fragmentation which has led to ignorance of patients’ concerns. This creates a linear and instrumental form of interaction in which many aspects of humanity are ignored. Figure 7 shows the overall features of a poor interaction between a doctor and a patient.
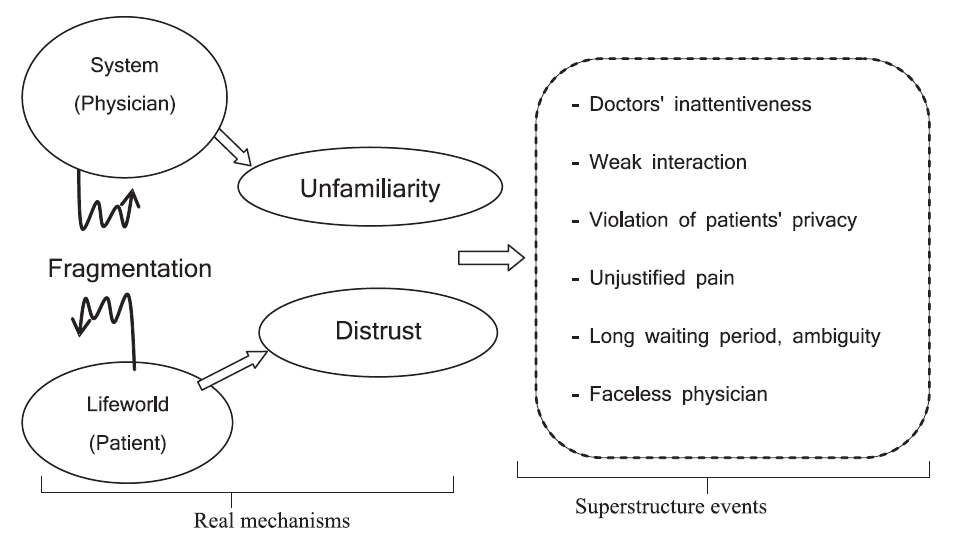
Figure 7 shows that the doctor–patient interaction occurs in a fragmented space. In this space, physicians are unfamiliar with patients’ lifeworld and this causes patients’ mistrust in the interaction. Consequently, the patient’s impression of the system becomes: doctors’ inattentiveness; weak interaction; invasion of patients’ privacy; unjustified pain; long waiting period, and ambiguity and faceless physician. As a result, doctors do not show sympathy towards patients’ lifeworld. In this situation, the patients’ lifeworld is ignored and suppressed by the unwritten laws of doctor–patient interactions.
As Cordella has mentioned, patients expect sympathetic and friendly communication from doctors. Listening, understanding, and answering patients’ questions with respect, support, reliability, patience and optimism are some features of sympathetic communication. Sympathetic communication should also include characteristics such as good verbal and non-verbal communication, to be a good listener, as well as have empathy (1).
Patients’ negative lived experiences are not only important for patients but they are also significant for healthcare providers and policy-makers. Therefore, models of patient-centredness and narrative medicine are recommended. These models consider patients’ needs as the main objective.
Limitations
One limitation of this study is an ethical one, involving participant observations. For ethical reasons, these observations were performed in a way that patients and their families did not know that the clinical supervisor is a researcher as well as a supervisor. Another limitation is with regards to the reasons why surgical patients were more dissatisfied. It seems that surgeons are more oblivious to patients’ expectations than other specialists. This aspect needs to be investigated further.
Conclusion
It seems that doctor-patient interactions in the context of this study were very weak. This led to negative experiences for patients and their families namely doctors’ inattentiveness; weak interaction; invasion of patients’ privacy; unjustified pain; long waiting period and ambiguity; and faceless physician. Due essentially to the unequal doctor-patient relationship, patients and their families feel that they are ignored, neglected and suppressed. Though the domination of the doctor is a characteristic of modern medicine, the problem is more severe in developing countries. Therefore, we recommend models of patient-centredness and narrative medicine. In addition, we recommend that the health system should monitor and evaluate the observance of ethics by physicians
Competing interests
The authors declare that they have no competing interests.
Acknowledgements
This study is extracted from the PhD dissertation of Ahmad Kelateh Sadati in Sociology titled Critical Narrative Analysis of Doctor–Patient Interaction in Shahid Faghihi Hospital approved (No.1069353) at Shiraz University. The research was a study to develop knowledge and does not seek to question the efforts of the physicians who are working against the clock to serve patients in this hospital. The researchers wish to thank all the participants in the study. The authors would also like to thank the Research Consulting Center of Shiraz University of Medical Sciences (RCC) for assistance in editing this article.
References
- Cordella M. The dynamic consultation: a discourse analytical study of doctor patient communication. John Benjamins Publishing; 2004.
- Kaba R, Sooriakumaran P. The evolution of the doctor–patient relationship. Int J Surg. 2007;5(1):57-65. Epub 2006 Mar 3.
- Kenny DA, Veldhuijzen W, Weijden Tv, Leblanc A, Lockyer J, Légaré F, Campbell C. Interpersonal perception in the context of doctor–patient relationships: a dyadic analysis of doctor–patient communication. Soc Sci Med. 2010;70(5):763-8. doi: 10.1016/j.socscimed.2009.10.065. Epub 2009 Dec 11.
- Liu X, Rohrer W, Luo A, Fang Z, He T, Xie W. Doctor–patient communication skills training in mainland China: a systematic review of the literature. Patient Educ Couns. 2015;98(1):3-14. doi: 10.1016/j.pec.2014.09.012. Epub 2014 Sep 30.
- Roter DL, Hall JA. Studies of doctor–patient interaction. Annu Rev Public health. 1989;10(1):163-80.
- Steihaug S, Gulbrandsen P, Werner A. Recognition can leave room for disagreement in the doctor–patient consultation. Patient Educ Couns. 2012;86(3):316-21. doi: 10.1016/j.pec.2011.06.011. Epub 2011 Jul 26.
- Kalateh Sadati A, Iman MT, Bagheri Lankarani K. Medical paraclinical standards, political economy of clinic, and patients’ clinical dependency: a critical conversation analysis of clinical counseling in South of Iran. Int J Community Based Nurs Midwifery. 2014;2(3):157-68.
- Sadati AK, Lankarani KB, Enayat H, Kazerooni AR, Ebrahimzadeh S. Clinical paternalistic model and problematic situation: a critical evaluation of clinical counseling. Journal of health sciences and surveillance system [JHSSS]. 2014;2(2):78-87.
- Pilnick A, Dingwall R. On the remarkable persistence of asymmetry in doctor/patient interaction: a critical review. Soc Sci Med. 2011;72(8):1374- 82. doi: 10.1016/j.socscimed.2011.02.033. Epub 2011 Mar 29.
- Parsons T. Social system. Routledge; 2013.
- Thompson MJ. Talcott Parsons and the logic of critical social theory. Situations: project of the radical imagination. 2012;4(2).
- Sadati AK, Lankarani KB, Afrasiabi H. Medical sociology; a neglected academic discipline in Iran. Shiraz E-Med J. 2015;16(5):e29224.
- Armstrong D. Bodies of knowledge/knowledge of bodies. In: Reassessing Foucault: power, medicine and the body. New York: Routledge, 1994.
- Driver F. Bodies in space: Foucault’s account of disciplinary power. In: Porter R, Jones C (eds). Reassessing Foucault: power, medicine and the body. Routledge; 1994, p. 113-31.
- Focault M. The birth of the clinic: an archeology of medical perception. New York: Vintage, 1975.
- Habermas J. The theory of communicative action. Volume 2: Lifeworld and system: a critique of functionalist reason. Beacon Press, 1985.
- Scambler G, Britten N. System, lifeworld and doctor-patient interaction: issues of trust in a changing world. In: Scambler G (ed). Habermas, critical theory and health. Routledge; 2001, Chapter 3, pp.45-67.
- Scambler G, Kelleher D. New social and health movements: issues of representation and change. Critical Public Health. 2006;16(3):219-31. DOI: 10.1080/09581590600986440.
- Mishler EG. The discourse of medicine: dialectics of medical interviews. Greenwood Publishing Group; 1984.
- Fairclough N. Discourse and social change. New York: Blackwell Publishing Inc;1992.
- Barry CA, Stevenson FA, Britten N, Barber N, Bradley CP. Giving voice to the lifeworld. More humane, more effective medical care? A qualitative study of doctor–patient communication in general practice. Soc Sci Med. 2001;53(4):487-505.
- Taylor SJ, Bogdan R. Introduction to qualitative research methods: the search for meaning. Wiley; 1984.
- Gold RL. Roles in sociological field observations. Social Forces. 1958;36(3):217-23. DOI: 10.2307/2573808.
- Fischer CT. Bracketing in qualitative research: conceptual and practical matters. Psychother Res. 2009;19(4-5):583-90. doi: 10.1080/10503300902798375.
- Carspecken PF. Critical ethnography in educational research: a theoretical and practical guide. Routledge; 1996.
- Carspecken PF. Critical ethnographies from Houston: distinctive features and directions. In: Carspecken PF, Walford G (eds). Critical ethnography and education (studies in educational ethnography, Volume 5). Emerald Group Publishing Limited; 2001, pp.1-26.
- Radigan J. The class clown and negotiated epistemology in a classroom. In: Carspecken PF, Walford G (eds). Critical ethnography and education (Studies in educational ethnography, Volume 5). Emerald Group Publishing Limited; 2001, pp.61-88.
- Mitchell G, Porter S, Manias E. A critical ethnography of communication processes involving the management of oral chemotherapeutic agents by patients with a primary diagnosis of colorectal cancer: study protocol. J Adv Nurs. 2015;71(4):922-32. doi: 10.1111/jan.12565. Epub 2014 Nov 10.
- Cook KE. Using critical ethnography to explore issues in health promotion. Qual Health Res. 2005;15(1):129-38.
- Batch M, Windsor C. Nursing casualization and communication: a critical ethnography. J Adv Nurs. 2015;71(4):870-80. doi: 10.1111/jan.12557. Epub 2014 Nov 6.
- American Sociological Association (ASA). Code of ethics and policies and procedures of the ASA Committee on Professional Ethics. American Sociological Association; 1999.
- Krleža-Jerić K, Lemmens T. 7th Revision of the Declaration of Helsinki: good news for the transparency of clinical trials. Croat Med J. 2009;50(2):105-10. doi: 10.3325/cmj.2009.50.105
- Atkinson P, Atkinson PA. Medical talk and medical work. The liturgy of the clinic. Sage Publications; 1995.
- Edwards G. Jurgen Habermas: politics and morality in health and medicine. In: Scambler G (ed). Contemporary theorists for medical sociology. New York: Routledge; 2012.
