THEME: TRUST IN HEALTHCARE
Development and testing of a scale to measure trust in the public healthcare system
Anand TN, V Raman Kutty
DOI: https://doi.org/10.20529/IJME.2015.044
Abstract
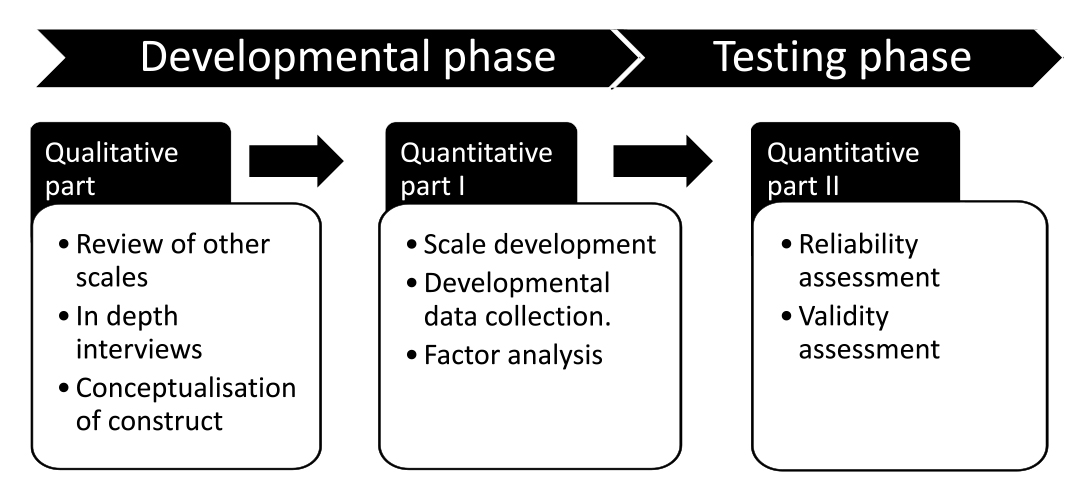
Trust is an important factor in improving the performance of the healthcare system. This study aimed to develop a validated scale to measure trust in the public healthcare system. We adopted a sequential exploratory mixed study design, with developmental and testing phases. In the developmental phase, the construct of “healthcare system trust” was conceptualised and items were generated on the basis of information from a review of the literature on trust, in-depth interviews and a review of other scales. Exploratory factor analysis was employed for item reduction. In the testing phase, the reliability and validity measures were established. The face validity, content validity and construct validity of the scale were assessed. The final scale was a Likert-type scale with 23 items, 16 of which measured trust in the healthcare providers and 7, in healthcare institutions. The scale is a valid and reliable tool for measuring trust in the public healthcare system.
Introduction
Trust is an essential factor in therapeutic relationships (1) and is described as the “lubricant of the social system” (2). Trust is operationally defined as the “optimistic acceptance of a vulnerable situation in which the truster believes the trustee will take care of the truster’s interests” (1). It is a combination of three components – the self, the specific partner, and a specific goal in a specific situation (3). Trust has two distinct elements: (i) interpersonal trust, which influences the day-to-day interactions between individuals, and (ii) social trust, which is developed through the collective actions of social institutions (1, 4).
The World Health Organization (WHO) defines a health system as “all actors, institutions and resources that undertake health actions – where a health action is one where the primary intent is to improve health” (5). A strong health system is an essential component of a healthy and equitable society (6). The health system is considered as a vital element in maintenance of the “health” of the community rather than as a mere delivery system (7).
Asymmetry in the spread of information and the unequal balance of power in the doctor–patient relationship augment the vulnerability of the patient (8). Trust in healthcare is defined as a “set of expectations that patients have from the healthcare system to help them heal; those expectations include appropriate diagnosis, correct treatment, non-exploitation, interest in the welfare of the patient and transparent disclosure of information” (9).Trust may be categorised according to the object of trust, ie it may be based on (i) individual trust (trust in an individual healthcare professional), or (ii) institutional trust (trust in a healthcare institution) (1, 10). The self-rated health condition of communities with higher levels of trust has been better than that of those with lower levels of trust (11, 12). Low levels of trust in the healthcare system eventually lead to perceptions of poor health, poor health outcomes and underutilisation of healthcare services (13, 14). They also inflate the cost associated with the sickness (7). A high level of trust in the healthcare provider is an indicator of the quality of healthcare (15). Technical competence, confidentiality, compassion, dependability, open communication and disclosure of information evoke trust (16, 17, 18, 19). A qualitative exploratory study conducted in India revealed that assurance of treatment, and loyalty to and respect for the physician are important dimensions of trust in a physician in the context of a developing country (20). Trust in the healthcare system reduces the risk of psychological distress among patients (21) and helps them to take more sound decisions regarding the treatment. Further, the level of the patients’ trust is of importance in the assessment of the performance of a healthcare organisation (22) or health system (23).
Scaling is a procedure which helps one to understand the level of a construct in each subject through the assignment of a score to specific levels of the construct or theoretical variable. Trust is conceptualised as a multidimensional construct and cannot be measured directly. Trust is difficult to measure since it depends upon the complex interaction between individual benefits and individual characteristics (24). Most of the scales available, measure trust in different components of the healthcare system.There are only a very few which measure trustinthe healthcare system as a whole (25). Measuring trust in the healthcare system helps to monitor trust and build a system which is considered more trustworthy and yields better health outcomes. Since each country has its unique health system, more precise results can be obtained if the scale for measuring trust is developed and tested in the very system in which it is intended to be used.
The rates of utilisation of healthcare depend on the people’s trust in the system. With the emergence of the private sector, there has been a decline in the utilisation of the public healthcare system and the cost of healthcare has increased. According to the Indian Human Development Survey, 2011–2012, the utilisation rates continued to fall even after the introduction of several programmes aimed at improving the utilisation of public healthcare facilities. Trust in the healthcare system, being an important determinant of healthcare utilisation, needs to be assessed in this context, hence the effort to develop a validated scale to measure trust in the public healthcare system.
The study aimed to develop a scale to measure trust in the healthcare system, and to test the scale for reliability and validity in the healthcare system of Kerala. It is well known that the performance of the health system in Kerala has been commendable. We also aimed to define the concept of “healthcare system trust”.
Methods
The study was conducted in two phases: Phase I (development of a scale) and Phase II (testing of the scale).
Study design: A sequential, exploratory, mixed study design was used. While developing the scale, qualitative and quantitative methods were adopted. In the testing phase, only quantitative methods were used.
Phase I: scale development
Conceptual model
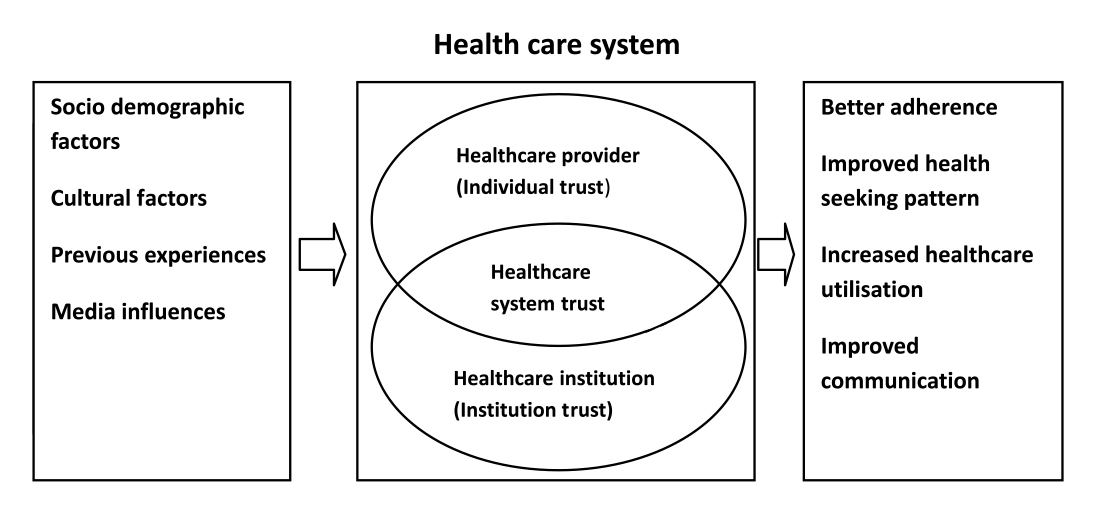
In this step, we operationally defined the construct “healthcare system trust”. The scales available now have been developed and tested chiefly in developed countries, where the structure of the healthcare system is entirely different from that in Kerala. A conceptual model was developed by integrating the healthcare distrust model with the information obtained from a review of the literature (26, 27, 28, 29, 30). In this model, trust in the healthcare system was defined as a combination of trust in the healthcare provider and trust in the healthcare institution. The elements which influence trust in the healthcare system included sociodemographic factors, previous experience with providers and institutions, cultural factors and exposure to the media.
In-depth interviews
Five in-depth interviews were conducted with adults who had used the public healthcare system in the previous three months. These were conducted on the basis of the in-depth interview guidelines, approved by the institutional ethics committee. The questions were based mainly on the information gathered from the review of the literature. Before the interviews, the participants were informed about the purpose of the study and their rights, and their written consent was sought.The purposive sampling method was adopted.We approached nine individuals, of whom five consented to participate. We conducted only five in-depth interviews because after that there was convergence of information.The place and time of interview were selected according to the informant’s preference. The interviews were conducted in the participant’s mother tongue (Malayalam). They started with a discussion of the general health status of the participants and moved on to questions related to trust in general, trust in the healthcare system, the qualities of trust worthy healthcare providers and experiences that improved trust in the healthcare system. In addition,the researcher also asked whether the respondents preferred public or private institutions. The interviews were recorded and transcribed in English by the researcher.The transcribed data were entered in Weft QDA version1.0.1 and coding of the interviews was done. Initially, open coding was done for one interview and it was on the basis of this that the other four interviews were coded. Themes were developed on the basis of these codes. These themes were merged with themes developed from the review of the literature. The assessment of the interviews provided various items that were important for the development of the scale.
Item generation and item pool creation
Items were generated with the help of the information collected from the review of the literature, in-depth interviews and review of the scales available. All the scales reviewed were designed to measure trust and most were used to measure “trust” in different settings.For the generation of items, we reviewed the Multidimensional Trust in Health Care Systems Scale (4),Trust in Primary Care Physician Scale (31), Trust in Physician Scale (19) and a scale measuring trust in a physician, a health insurer and the medical profession (32). In addition, we reviewed many studies assessing trust in relation to healthcare (20, 33, 34, 35). An initial item pool consisting of 40 items was translated into Malayalam and back into English. The translated version was submitted to an independent party to be checked for language errors.
Item reduction
Item reduction was done in three steps. Initially, each item was evaluated and prioritised by an expert. Next, item reduction was achieved on the basis of item to total correlation analysis and exploratory factor analysis. We adopted exploratory factor analysis because no perfect theory has been developed on trust in the healthcare system. For factor analysis, a sample size of 200 is considered adequate (36) and a sample size of 150 is used in scale development approaches (37). In this study, we considered 200 an appropriate sample size for factor analysis. We adopted a purposive sampling strategy to recruit an equal proportion of males and females. The preliminary scale was administered to a sample of 200 subjects of the ages of 18–55 years. We approached the subjects in their homes, which were located in the Kalloorkad panchayat in Kerala.
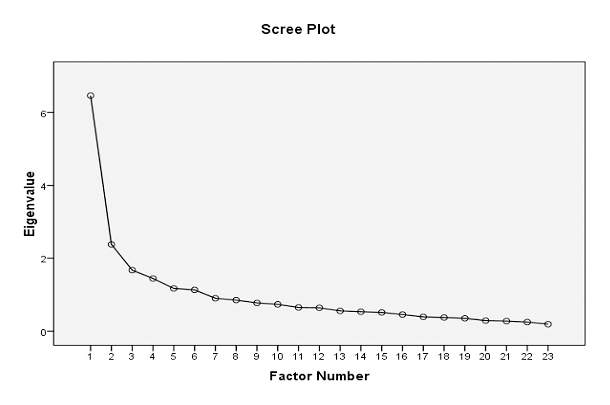
The preliminary scale was administered to 200 subjects who had used public health facilities within the three months before the interview. Their consent was obtained prior to the collection of data. The socio-demographic details of the sample were also gathered during the collection of the data. We adopted the maximum likelihood method for factor extraction. To identify the number of factors to be retained, we used eigen values and a scree plot. Items with eigen values of more than one were retained for rotation and in thescree plot, all factors above “elbow point” were retained for rotation. We adopted the oblique rotation method because most factors are correlated (38). Data entry was done using the Epidata (3.1 Version) software. The data were analysed using the SPSS (21.0) IBM software.
Phase II: testing of the scale
Reliability
We adopted two methods of assessing reliability: internal consistency reliability and test retest reliability. Internal consistency was measured using Cronbach’s alpha coefficient. The data collected from the developmental sample were used for this purpose. The test retest reliability assessment was done by administering the scale to the same sample on two different occasions, ie to 20 adults of the ages of 18–55 years, on two occasions separated by a gap of seven days.
Validity
The scale was subjected to three forms of validity measurement: face validity, content validity and construct validity. Face validity was ensured by subjecting the scale to examination by experts in the field. The Malayalam and English versions were submitted to 10 public health experts to ensure that the translations were right. Content validity was calculated by submitting the scale to experts for review. Ten public health experts were requested to evaluate and review the scale, and to rate each item according to its necessity in the scale. We adopted the Lawshe (39) method of calculating the content validity ratio and content validity index.
Construct validity was established by assessing the scale for convergent and divergent validity. Convergent validity was calculated by correlating the scores obtained from the General Trust Scale (40) and the newly developed public healthcare system trust scale. Since the two constructs have similar characteristics, they should be correlated. Divergent validity was calculated by correlating the scores from the short form of the Medical Mistrust Index (41) and the newly developed public healthcare system trust scale. Since these two constructs are theoretically opposite, their scores should be negatively correlated.
Ethical clearance was obtained from the institutional ethics committee of the Sree Chitra Tirunal Institute for Medical Sciences and Technology, Trivandrum.
Results
Phase I: scale development
In-depth interviews: In-depth interviews were used to understand how people generally define the word “trust”. They also helped to understand their ideas regarding the “healthcare system” and “healthcare system trust”. The informants described the experiences they had had while utilising the public healthcare system and the qualities they expecteda trustworthy healthcare provider, as well as a trustworthy healthcare institution, to have. The participants recollected incidents that fostered or reduced their trust in the public healthcare system, and compared the performance of different government departments, such as the public education system and public healthcare system.
The respondents defined the word “trust” as follows:
“Trust means the trustee will not harm the truster and the trustee will protect the truster in all situations from harm”
According to the respondents, the characteristics of general trust were dependability, honesty, transparency in relations and the ability to understand people. The informants defined “healthcare system trust” as a combination of trust in the healthcare provider (doctor, nurse or other), the healthcare institution and the quality of drugs. According to the participants, there should be transparency in the transactions between healthcare professionals and individuals.
Information regarding the diagnosis or treatment should be communicated appropriately to the patient. Effective communication is necessary to build trust between the two parties. The participants identified two components of healthcare services: healthcare providers and healthcare institutions. However, they were not familiar with the concept of “healthcare system”. During the interviews, the informants said that trust in the healthcare system “is developed and influenced by the interactions between individuals and professionals in the healthcare system”.
This information emphasises the contribution of trust in the healthcare provider (individual trust) towards trust in the healthcare system.
One of the qualities that makes a healthcare provider trustworthy is “patience”. The informants expected their healthcare providers to listen to them patiently. They also expected them to be “empathetic”, “efficient” and “assertive”, and to have “good knowledge”. In addition, the informants felt that there should be a personal element in the interaction with the healthcare provider. Healthcare professionals were expected to know about the medical, as well as economic and social, conditions of the client. The participants mentioned that they would trust healthcare professionals who were not profit-oriented.
According to the informants, public healthcare institutions should deliver quality services, otherwise the people’s trust in the public healthcare system would be affected. They should be well managed, and should provide quality drugs and treatment at a reasonable cost. Public healthcare institutions should have an adequate number of employees. Also, they should be dependable and reliable. In the words of one informant
“Since two of our PHC staff stay near, we have always a place to go when we have any health problems and they provide us good service with very little expense.”
According to the informants, previous experiences and the media did have an influence on the people’s trust in healthcare institutions.They described experiences they had had with healthcare providers and healthcare institutions that had altered their level of trust. For a healthcare provider to be trustworthy, he/she should have “kaipunyam“, which means that he/she should be competent enough to prevent, diagnose and treat a disease correctly. Most participants attached importance to the way the healthcare provider addressed them; if the latter addressed them by their names, they were more likely to trust him/her. The participants preferred to be identified by their names rather than an impersonal number.
During the interview we compared the performance of the public education system and the public healthcare system. Three of the five participants felt that the performance of the public education system was better than that of the public healthcare system. According to them, this was because the health department was short of funds. Four participants preferred private health facilities because they believed that there would not be any delays in treatment in these facilities. Further, many private facilities had all the resources required to treat diseases.
Item reduction
The initial item pool had 40 items. Following evaluation by experts, eight were removed to form a 32-item Likert-type scale with five responses ranging from “Strongly disagree” to “Strongly agree”. The preliminary scale with 32 items was administered to 200 individuals and the data were collected. In addition, we collected the sociodemographic data of the subjects.
In the scale development sample, 49.5% of the subjects were above the poverty line and 58.5% preferred private healthcare facilities over public healthcare facilities. The mean age of the participants was 37.53±9.47 years. The data collected using the preliminary scale were used for calculating internal consistency. In this step, one item was removed because item removal leads to an improvement in Cronbach’s alpha value. Thus, it became a 31-item scale. Exploratory factor analysis was done for this scale, with a Cronbach’s alpha of 0.877.Factor analysis showed eight factors with eigen values of more than one and covering 52.33% of the scale variance. Items showing negative loading and cross-loading were removed. (Cross-loading occurs when one item loads on different factors with a value of 0.32 or more) (42). Cross-loading made the factor structure unstable, so eight items were removed from the 31-item scale to forma 23-item scale. After the revision, a 6-factor structure evolved from factor analysis and it covered 51.46% of the scale variance, with a Cronbach’s alpha of 0.866. The scree plot also revealed a 6-factor structure. The elbow point in a scree plot denotes the number of factors.
| Table 1: Characteristics of study participants in developmental sample (n=200) | ||
|
Characteristics |
Categories |
Frequency (percentage) |
|
Age |
18–25 years 26–35 years 36–45 years 46–55years |
18 (9.0) 67 (33.5) 66 (33.0) 49 (24.5) |
|
Sex |
Male Female |
90 (45.0) 110 (55.0) |
|
Education |
No formal education Primary school High school Higher secondary Graduate Postgraduate and above |
3 (1.5) 39 (19.5) 59 (29.5) 50 (25.0) 42 (21.0) 7 (3.5) |
|
Occupation |
Unemployed |
13 (6.5) |
|
Self-employed |
52 (26.0) |
|
Labourer |
30 (15.0) |
|
Government employee |
22 (11.0) |
|
Home-maker |
48 (24.0) |
|
Agriculture |
11 (5.5) |
|
Service sector |
14 (7.0) |
|
Student |
10 (5.0) |
There was a minimum communality of 0.20. More than five variables loaded strongly, with a maximum loading value of 0.70 and a minimum of 0.30. The results of the factor analysis were a 23-item scale with six underlying factors, covering 51.46% of the variance.
The following is the pattern matrix that shows which items cling together to form a factor.
| Table 2: Pattern matrix – factor loading of scale items in factor analysis | |||||||
| No. | Items | Factors | |||||
| 1 | 2 | 3 | 4 | 5 | 6 | ||
| 1 | My healthcare institution provides me quality care. | 0.409 | |||||
| 2 | The treatment expenses in my healthcare institution are reasonable. | 0.994 | |||||
| 3 | I think I can tell my healthcare provider everything, so that he/she can understand my condition better. | 0.993 | |||||
| 4 | My healthcare provider understands my economic and social conditions. | 0.485 | |||||
| 5 | I believe my healthcare provider is efficient in terms of using the available resources. | 0.476 | |||||
| 6 | Even if my healthcare provider makes a mistake, I believe in him/her. | 0.683 | |||||
| 7 | My healthcare provider gives value to my time also during consultation. | 0.503 | |||||
| 8 | My healthcare institution has all the latest facilities for diagnosis and treatment. | 0.504 | |||||
| 9 | I believe my healthcare institution has enough employees for providing health services. | 0.471 | |||||
| 10 | I have never taken a second opinion from health workers about my health problem. | 0.471 | |||||
| 11 | My healthcare provider listens to me patiently about my health problems. | 0.760 | |||||
| 12 | My healthcare provider considers every patient equal. | 0.468 | |||||
| 13 | Often, I feel that my healthcare provider maintains confidentiality. | 0.648 | |||||
| 14 | I believe that my healthcare provider will give me the right treatment. | 0.430 | |||||
| 15 | My healthcare provider will give me all the information available on the diagnosis and treatment of my illness. | 0.667 | |||||
| 16 | My healthcare provider will involve me in the decision-making process regarding my treatment. | 0.727 | |||||
| 17 | I believe that I can approach my healthcare institution for any medical problem. | 0.747 | |||||
| 18 | I recommend my healthcare institutionto my friends. | 0.659 | |||||
| 19 | My healthcare institution is a dependable one. | 0.821 | |||||
| 20 | I believe my healthcare providers are technically competent. | 0.658 | |||||
| 21 | I often try to follow the instructions my healthcare provider gives me. | 0.547 | |||||
| 22 | I respect my healthcare provider for his/her activities. | 0.398 | |||||
| 23 | I believe that the health promotional messages given by my healthcare provider are valid and logical. | 0.333 | |||||
From the pattern matrix, we identified six factors. Each of these was assigned to one domain of the construct of “healthcare system trust”. The domains were identified with the help of a review of the literature and in-depth interviews. The factor structure thus formed was close to the conceptual framework of the construct of “healthcare system trust”
| Table 3: Factors showing characteristics of different domains | |||
| No. | Factors | Component of health system trust | Domain |
| 1 | Factor 1 | Institutional trust | Quality |
| 2 | Factor 2 | Individual trust | Communication |
| 3 | Factor 3 | Overlapping* | — |
| 4 | Factor 4 | Individual trust | Transparency |
| 5 | Factor 5 | Institutional trust | Reliability |
| 6 | Factor 6 | Individual trust | Competency |
| Annexure I: Factor correlation matrix | ||||||
| Factor | 1 | 2 | 3 | 4 | 5 | 6 |
| 1 | 1.000 | 0.133 | 0.180 | 0.190 | 0.271 | 0.185 |
| 2 | 0.133 | 1.000 | 0.108 | 0.119 | 0.141 | 0.197 |
| 3 | 0.180 | 0.108 | 1.000 | 0.275 | 0.476 | -0.027 |
| 4 | 0.190 | 0.119 | 0.275 | 1.000 | 0.197 | 0.191 |
| 5 | 0.271 | 0.141 | 0.476 | 0.197 | 1.000 | -0.004 |
| 6 | 0.185 | 0.197 | -0.027 | 0.191 | -0.004 | 1.000 |
| Annexure II: Public healthcare system trust scale | ||||
| Healthcare provider trust (individual trust) | ||||
| No | Item | Item statistics | ||
| Mean | Std. deviation | N | ||
| 1 | I believe my healthcare provider is technically competent. | 4.08 | 0.63 | 200 |
| 2 | My healthcare provider will give all the information available on the diagnosis and treatment of my illness. | 3.80 | 0.62 | 200 |
| 3 | I believe that my healthcare provider will give me the right treatment. | 3.96 | 0.41 | 200 |
| 4 | My healthcare provider understands my economic and social conditions. | 3.04 | 1.13 | 200 |
| 5 | I believe my healthcare provider is efficient in terms of using the resources available. | 3.66 | 0.80 | 200 |
| 6 | I often try to follow the instructions my healthcare provider gives me. | 3.82 | 0.62 | 200 |
| 7 | I have never taken a second opinion from health workers about my health problem. | 3.42 | 0.95 | 200 |
| 8 | Even if my healthcare provider makes a mistake, I believe in him/her. | 2.36 | 1.19 | 200 |
| 9 | My healthcare provider gives value to my time also during consultation. | 3.15 | 0.97 | 200 |
| 10 | I believe that the health promotional messages given by my healthcare provider are valid or logical. | 3.78 | 0.64 | 200 |
| 11 | My healthcare provider listens to me patiently about my health problems. | 3.38 | 0.94 | 200 |
| 12 | I think I can tell my healthcare provider everything, so that he/she can understand my condition better. | 3.82 | 0.60 | 200 |
| 13 | My healthcare provider considers every patient equal. | 3.35 | 0.97 | 200 |
| 14 | My healthcare provider will involve me in the decision-making process regarding my treatment | 3.60 | 0.71 | 200 |
| 15 | Often, I felt that my healthcare provider maintains confidentiality. | 3.12 | 0.92 | 200 |
| 16 | I respect my healthcare provider for his/her activities. | 4.14 | 0.55 | 200 |
| Healthcare institution trust (institutional trust) | ||||
| 17 | My healthcare institution has all the latest facilities for treatment and diagnosis. | 3.14 | 1.18 | 200 |
| 18 | The treatment expenses in my healthcare institution are reasonable. | 3.76 | 0.62 | 200 |
| 19 | My healthcare institution provides me quality care. | 3.76 | 0.68 | 200 |
| 20 | I believe my healthcare institution has enough employees for providing health services | 3.00 | 1.33 | 200 |
| 21 | I recommend my healthcare institution to my friends. | 3.59 | 0.76 | 200 |
| 22 | My healthcare institution is a dependable one. | 3.68 | 0.72 | 200 |
| 23 | I believe that I can approach my healthcare institution for any medical problem. | 3.71 | 0.72 | 200 |
Phase II: testing of the scale
Reliability
Internal consistency was assessed from the developmental sample. Cronbach’s alpha value for the final scale was 0.86. For standardised items, Cronbach’s alpha value was 0.85. The test retest reliability was estimated by administering the 23-item scale to 20 individuals of 18–55 years of age, with a gap of seven days. The scores of the two tests were correlated (r= 0.97,p<0.05). The correlation for each item was also calculated; all of them were positively correlated.
Validity
Face validity was established by submitting the formatted and translated version of the scale to 10 experts in the public health domain. The experts assessed the scale for the adequacy of its content and sufficiency of the items. The content validity ratio ranged from 0.62 to 0.73. The content validity index, calculated as the mean value of the content validity ratios, was 0.64.
Construct validity was established by assessing convergent and divergent validity. Convergent validity was assessed by correlating the scores obtained in the public healthcare system trust scale with those obtained in the general trust scale. There was a significant correlation between the scores in the two scales, with the correlation coefficient being (r=0.48, p<0.05). Divergent validity was measured by testing the correlation between the scores obtained in the Medical Mistrust Index and public healthcare system trust scale. The two scores were negatively correlated the correlation coefficient being (r=-0.52, p<0.05).
The mean public healthcare system trust scale score for the developmental sample was 81.24±9.81, with a range of 58–104. Further analysis revealed that there was no statistically significant difference between the mean scores on the basis of age, education and economic status. However, there was a significant difference between the total mean scores of males and females, and the employed and unemployed.
| Table 4: Mean public healthcare system trust scale score by sample characteristics in developmental sample | ||
| Sample characteristics(n=200) | Mean±SD | p value |
| Age
18–37 years 38–55 years |
81.27±9.52 81.29±10.06 |
0.98 |
| Sex
Male Female |
77.79±8.46 84.07±9.96 |
<0.05 |
| Education
Upto high school Above high school |
82.13±10.63 80.34±8.85 |
0.19 |
| Occupation
Unemployed Employed |
85.69±8.94 78.80±9.42 |
<0.05 |
| Economic status
Above poverty line Below poverty line |
81.26±9.97 81.23±9.69 |
0.98 |
Discussion
The newly developed public healthcare system trust scale is intended to measure the trust in the public healthcare system. It was developed through review of the literature and qualitative exploration of the construct of “healthcare system trust”. The study demonstrated the multidimensionality of the construct. This corresponds with the findings of previous studies (4, 20).
The participants’ ideas of “trust” were closely related to the literature on trust and the theories on the subject (43, 44). Importantly, according to them, trust in the healthcare system had two components: trust in the healthcare provider and trust in the healthcare institution. The data from the in-depth interviews emphasise the contribution of trust in the healthcare provider (individual trust) towards trust in the system. Due to the limitation of time, we were unable to fully explore the concept of trust in the healthcare system. We were able to touch only the surface of this complex construct. Judging by the qualitative exploration, it appeared that “healthcare system trust” is closely linked with what people perceive of as “quality”, “reliability” and “continuity” in healthcare.
In this study, we identified five domains of the construct of”healthcare system trust”: perceived quality of services, effective communication, transparency in relations, reliability and technical competence. These domains are different from those identified by previous studies. This may be attributed to the overlapping factors in the structure and the complexity of theconstruct. A close examination of factor 3 resulted in the identification of additional domains, which were economic dependability, loyalty, comfort, confidentiality and acceptance of providers’ drawbacks (20, 45, 46). Confidentiality was not identified as a major domain in this scale, but it was present in item 13 (“I feel that my healthcare provider maintains confidentiality”). In previous studies, “honesty” and “veracity” have been found to be an important domain of trust (46). However, they can probably be incorporated into the domains of loyalty, competency and transparency. Due to the structure of this scale, ie a structure with overlapping factors, there is a need for further research on the construct "healthcare system trust".
The newly developed public healthcare system trust scale is unique to a Kerala context and it differs from other scales measuring trust. The Multidimensional Trust in Healthcare Systems Scale also measures trust in the healthcare system. However, in this scale,the foci of trust are the healthcare provider, healthcare institution and healthcare payer (4). In our study, we did not include the healthcare payer because the cost of treatment is borne mostly by the patients themselves. The two scales have been constructed to measure trust in different conditions – one in developed countries and the other in developing countries.
Among the items, item 22 (“I respect my healthcare provider”) received the highest individual item mean score. Item 6 (“Even if my healthcare provider makes a mistake, I believe in him/her”) received the lowest individual item mean score. Item 12 (“My healthcare provider considers every patient equal”) was a unique item in this scale. It is featured under the additional domain of “comfort” in factor 3.This item implies that any type of discrimination on the provider’s part will affect the level of trust. Item 21 (“I often try to follow the instructions my healthcare provider gives me”) suggests a link between adherence and trust in the healthcare system (47).
The Cronbach’s alpha value of the newly developed scale was 0.86, which shows high internal consistency. This indicates how well a number of items converge on one construct. A value above 0.70 is considered adequate (48). As Cronbach’s Alpha value is proportional to number of items, a high alpha value is possible even if the construct is multidimensional (49). The Cronbach’s alpha value of similar scales measuring trust in the healthcare system ranges from 0.75–0.95.The new trust scale identified six factors and the Cronbach’s alpha value of these factors ranged from 0.61–0.86.The reliability of the scale was enhanced and proven with test retest reliability (25).
To assess the validity of the construct, we adopted convergent and divergent validity measurement. To establish construct validity, we used two constructs – general trust and medical mistrust.Other scales measuring trust in the healthcare system have used scales assessing constructs such as patient-centred care, adherenceto medication, patients’ satisfaction and social support (4). A review of the scales for trust in the healthcare system showed that to validate the scale, the constructs used most often included quality, satisfaction, financial factors and equity (25).
The public healthcare system trust scale revealed a statistically significant difference between the level of trust among males and females (50). Females had a higher trust score than males. The trust scores were significantly different for the employed and unemployed groups, being higher among the latter than the former. This difference could perhaps be attributed to variation in certain other factors, such as exposure to the media, economic independence and social interaction (35, 51, 52). The analysis of the developmental sample scores was incapable of explaining the variation across different variables. A multivariate analysis was essential to explain the interaction between the variables and trust, but the analysis was restricted due to the small sample size. More studies are needed to validate these findings.
Strengths and limitations of the study
The study produced a valid and reliable tool for measuring trust in the public healthcare system. The strength of the study was its use of exploratory factor analysis for item reduction and the identification of the factors. The study was able to establish three types of validity for the scale. It identified trust in the healthcare provider (individual trust) and trust in the healthcare institution (institutional trust) as the major components of trust in the public healthcare system in Kerala – a finding which is similar to those of research conducted in this area earlier (4). The main limitation of the scale was that it used an individual item scoring method. The total score of the scale was calculated as the sum of the scores of the individual items. This might have resulted in the neglect of the specific contribution of individual items. The other limitations included the structure, which was characterised by overlapping factors, and the limited variability of the developmental sample.
Public health implications
The public healthcare system trust scale can be used as a surrogate measure of the quality of the health services provided by the public healthcare system, since quality and trust are highly correlated. Trust in the healthcare system is an important determinant of health at present. Trust in the healthcare system is associated with health outcomes. This fact should be considered while developing policies which aim to improve the utilisation of healthcare. Policies aiming to improve communication between people and health professionals should consider the communicative aspects of trust, which have their own role to play in producing better health outcomes.
Competing interests: The authors report no competing interests.
Funding: The study was funded by Health System Research India Initiative, Trivandrum, Kerala. It has not been submitted for publication elsewhere.
Acknowledgements
We thank Dr Vijayaprasad Gopichandran, Assistant Professor, ESIC Medical College and PGIMSR, Chennai, and Dr Jagadish Khubchandani, Assistant Professor of Community Medicine, Ball State University, Muncie, for their guidance and support.
References
- Hall MA, Dugan E, Zheng B, Mishra AK. Trust in physicians and medical institutions: what is it, can it be measured, and does it matter? Milbank Q. 2001[cited 2015 June 23];79(4):613-39, v. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2751209&tool=pmcentrez&rendertype=abstract.
- Arrow KJ. The Limits of organization. New York: WW Norton; 1974. p 23.
- Simpson, JA. Psychological foundations of trust. Curr Dir Psychol Sci. 2007[cited 2015 June 23];16(5):264-8.Available from: http://cdp.sagepub.com/content/16/5/264.abstract.
- Egede LE, Ellis C.Development and testing of the Multidimensional Trust in Health Care Systems Scale. J Gen Intern Med. 2008[cited 2014 Feb 13];23(6):808-15. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2517872&tool=pmcentrez&rendertype=abstract
- World Health Organization 2000. The World Health Report 2000 [Internet]. Health systems: Improving performance [cited 2015 June 23]. Available from: http://www.who.int/whr/2000/en/whr00_en.pdf.
- Backman G, Hunt P, Khosla R, Jaramillo-Strouss C, Fikre BM, Rumble C, Pevalin D, Páez DA, Pineda MA, Frisancho A, Tarco D, Motlagh M, Farcasanu D, Vladescu C. Health systems and the right to health: an assessment of 194 countries. Lancet. 2008[cited 2014 Jun 1] ;372(9655):2047-85. Available from: http://www.sciencedirect.com/science/article/pii/S014067360861781X.
- Gilson L. Editorial: building trust and value in health systems in low- and middle-income countries. Soc Sci Med 2005[cited 2014 Feb 15] ;61(7):1381-4. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16005773.
- Goold SD. Trust, distrust and trustworthiness. J Gen Intern Med. 2002 [cited 2015 June 10]. ;17(1):79-81. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1495000&tool=pmcentrez&rendertype=abstract.
- Caterinicchio R. Testing plausible path models of interpersonal trust in patient physician treatment relationships. SocSci Med. 1979;13:81-99.
- Hardin R. Conceptions and explanations of trust. In: Cook KS (ed). Trust in Society. New York: Russell Sage Foundation; 2001:3-40.
- Jen MH, Sund ER, Johnston R, Jones K.Trustful societies, trustful individuals, and health: An analysis of self-rated health and social trust using the World Value Survey. Health Place.2010[cited 2014 Feb 15] ;16(5):1022-9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20621543.
- Giordano GN, Lindstrom M. The impact of changes in different aspects of social capital and material conditions on self-rated health over time: a longitudinal cohort study. SocSci Med. 2010[cited 2014 Feb 12]. ;70(5):700-10. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20022681.
- Radin D. Does corruption undermine trust in health care? Results from public opinion polls in Croatia. Soc Sci Med. 2013 [cited 2014 Jun 15].;98:46-53. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24331881.
- Mohseni M, Lindstrom M. Social capital, trust in the health-care system and self-rated health: the role of access to health care in a population-based study. Soc Sci Med. 2007[cited 2014 Jan 29]. ;64(7):1373-83. Available from: http://www.ncbi.nlm.nih.gov/pubmed/17202025.
- Gopichandran V, Chetlapalli SK. Factors influencing trust in doctors: a community segmentation strategy for quality improvement in healthcare. BMJ Open. 2013b [cited 2014 Jun 7] ;3(12):e004115]. Available from: http://bmjopen.bmj.com/content/3/12/e004115.full.
- Russell S. Treatment-seeking behaviour in urban Sri Lanka: trusting the state, trusting private providers. SocSci Med. 2005[cited 2014 May 28]. ;61(7):1396-407. Available from: http://www.sciencedirect.com/science/article/pii/S0277953604006641.
- Mechanic D. The functions and limitations of trust in the provision of medical care. J Health Polit Policy Law, 1998[cited 2015 June 10] ;23(4):661-86. Available from: http://www.ncbi.nlm.nih.gov/pubmed/9718518.
- Emanuel EJ, Dubler NN. Preserving the physician-patient relationship in the era of managed care. JAMA. 1995;273(4):323-9[cited 2015 June 10]. Available from: http://www.ncbi.nlm.nih.gov/pubmed/7815662.
- Anderson LA, Dedrick RF. Development of the Trust in Physician scale: a measure to assess interpersonal trust in patient-physician relationships. Psychol Rep. 1990;67(3 Pt 2):1091-100[cited 2015 June 10]. Available from: http://www.ncbi.nlm.nih.gov/pubmed/2084735.
- Gopichandran V, Chetlapalli SK. Dimensions and determinants of trust in health care in resource poor settings—a qualitative exploration. PLoS One. 2013a [cited 2014 Jan 22];8(7):e69170. Available from: http://dx.plos.org/10.1371/journal.pone.0069170.
- Ahnquist J, Wamala SP, Lindström M. What has trust in the health-care system got to do with psychological distress? Analyses from the national Swedish survey of public health. Int J Qual Health Care. 2010[cited 2014 June 3]. ;22(4):250-8. Available at: http://intqhc.oxfordjournals.org/content/22/4/250.full.
- Goold SD. Trust and the ethics of health care institutions. Hastings Cent Rep. 2001 [cited 2014 Jun 9].;31(6):26-33. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12945452.
- Gilson L. Trust and the development of health care as a social institution. SocSci Med. 2003;56(7):1453-68[cited 2015 June 23]. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12614697.
- Gopichandran V, Wouters E, Chetlapalli SK. Development and validation of a socioculturally competent trust in physician scale for a developing country setting. BMJ Open. 2015;5(4):e007305[cited 2015 May 13]. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=4420938&tool=pmcentrez&rendertype=abstract.
- Ozawa S, Sripad P. How do you measure trust in the health system? A systematic review of the literature. SocSci Med. 2013;91:10-14[cited 2014 February 12]. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23849233.
- Armstrong K, Rose A, Peters N, Long JA, McMurphy S, Shea JA. Distrust of the health care system and self-reported health in the United States. J Gen Intern Med. 2006 [cited 2014 June 14];21(4):292-7. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1484714&tool=pmcentrez&rendertype=abstract.
- Trachtenberg F, Dugan E, Hall MA. How patients’ trust relates to their involvement in medical care. J FamPract. 2005[cited 2014 Feb 21]. ;54(4):344-52. Available from: http://www.ncbi.nlm.nih.gov/pubmed/15833226.
- Bonds DE, Camacho F, Bell RA, Duren-Winfield VT, Anderson RT, Goff DC.The association of patient trust and self-care among patients with diabetes mellitus. BMC FamPract. 2004 [cited 2014 Feb 21].;5:26. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=535564&tool=pmcentrez&rendertype=abstract.
- Gilson L, Palmer N, Schneider H. Trust and health worker performance: exploring a conceptual framework using South African evidence. SocSci Med. 2005[cited 2014 Jun 7] ;61(7):1418-29. Available from: http://www.sciencedirect.com/science/article/pii/S027795360400646X.
- O’Malley AS, Sheppard VB, Schwartz M, Mandelblatt J.The role of trust in use of preventive services among low-income African-American women. Prev Med.2004 [cited 2014 May 28].;38(6):777-85. Available from: http://www.sciencedirect.com/science/article/pii/S0091743504000416.
- Hall MA, Zheng B, Dugan E, Camacho F, Kidd KE, Mishra A, Balkrishnan R.Measuring patients’ trust in their primary care providers. Med Care Res Rev. 2002[cited 2014 Feb 10]. ;59(3):293-318. Available from: http://mcr.sagepub.com/cgi/doi/10.1177/1077558702059003004.
- Dugan E, Trachtenberg F, Hall MA. Development of abbreviated measures to assess patient trust in a physician, a health insurer, and the medical profession. BMC Health Ser Res. 2005[cited 2015 Jun 11]. ;5:64. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1262715&tool=pmcentrez&rendertype=abstract.
- Dinç L, Korkmaz F, Karabulut E. A validity and reliability study of the multidimensional trust in health-care systems scale in a Turkish patient population. Soc Indic Res. 2012 [cited 2014 Mar 4].;113(1):107-120. Available from: http://link.springer.com/10.1007/s11205-012-0084-y.
- Mechanic D, Meyer S. Concepts of trust among patients with serious illness. SocSci Med. 2000[cited 2015 Jun 23]. ;51(5):657-68. Available from: http://www.ncbi.nlm.nih.gov/pubmed/10975226.
- Tokuda Y, Fujii S, Jimba M, Inoguchi T. The relationship between trust in mass media and the healthcare system and individual health: evidence from the Asia Barometer Survey. BMC Med. 2009 [cited 2014 Feb 5];7:4. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2655302&tool=pmcentrez&rendertype=abstract.
- Floyd F, Widaman KF. Factor analysis in the development and refinement of clinical assessment instruments. Psychological Assessment. 1995 [cited 2015 Jun 23];7(3):286-99. Available from: http://psycnet.apa.org/psycinfo/1996-93316-001.
- DeVellis RF. Scale development: theory and applications. SAGE Publications; 1991[cited 2014 Feb 16]. Available at: http://books.google.com/books?hl=en&lr=&id=Rye31saVXmAC&pgis=1.
- Donald R. An alternative procedure for assessing convergent and discriminant validity. Appl Psychol Meas. 1988 [cited 2015 Jun 23].;12(4):411-23. Available from: http://conservancy.umn.edu/bitstream/handle/11299/104316/v12n4p411.pdf?sequence=1&isAllowed=y.
- DeVon HA, Block ME, Moyle-Wright P, Ernst DM, Hayden SJ, Lazzara DJ, Savoy SM, Kostas-Polston E.A psychometric toolbox for testing validity and reliability. J Nurs Scholarsh. 2007[cited 2015 Jun 23]. ;39(2):155-64. Available from: http://www.ncbi.nlm.nih.gov/pubmed/17535316.
- Yamagishi T, Yamagishi M. Trust and commitment in the United States and Japan. Motiv Emot. 1994[cited 2015 Jun 23] ;18(2):129-66. Available from: http://www.researchgate.net/profile/Toshio_Yamagishi/publication/225182584_Trust_and_commitment_in_the_United_States_and_Japan/links/0c96052705d9fdadd7000000.pdf.
- LaVeist TA, Isaac LA, Williams KP. Mistrust of health care organizations is associated with underutilization of health services. Health Serv Res. 2009 [cited 2015 Jul 6].;44(6):2093-105. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2796316&tool=pmcentrez&rendertype=abstract
- Clark LA, Watson D. Constructing validity: basic issues in objective scale development. Psychological Assessment. 1995[cited 2015 Jun 23] ;7(3):309-19]. Available from: http://www.personal.kent.edu/~dfresco/CRM_Readings/Clark_and_Watson_1995.pdf.
- Müller E, Zill JM, Dirmaier J, Härter M, Scholl I. Assessment of trust in physician: a systematic review of measures. PLoS One. 2014[cited 2015 Jun 11] ;9(9):e106844 Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4160203/?tool=pmcentrez.
- Ward P. Trust, reflexivity and dependence: A “social systems theory” analysis in/of medicine. European Journal of Social Quality. 1995[cited 2015 Jun 23] ;6(2):143-58 Available from: http://www.jstor.org/stable/23971853.
- Straten GFM, Friele RD, Groenewegen PP. Public trust in Dutch health care. Soc Sci Med. 2002[cited 2015 Jun 11] ;55(2):227-34 Available from: http://www.ncbi.nlm.nih.gov/pubmed/12144137.
- Hall MA, Camacho F, Dugan E, Balkrishnan R.Trust in the medical profession: conceptual and measurement issues. Health Serv Res. 2002[cited 2015 Jun 11] ;37(5):1419-39. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1464022&tool=pmcentrez&rendertype=abstract.
- Altice FL, Mostashari F, Friedland GH. Trust and the acceptance of and adherence to antiretroviral therapy. J Acquir Immune Defic Syndr. 2001Sep 1 [cited 2015 June 12];28(1):47-58. Available from: http://www.ncbi.nlm.nih.gov/pubmed/11579277.
- Grau E. Using factor analysis and Cronbach’s alpha to ascertain relationships between questions of a dietary behavior questionnaire. Section on Survey Research Methods. 2007[cited 2015 Jun 23]:3104-10. Available from: http://www.amstat.org/sections/srms/proceedings/y2007/Files/JSM2007-000505.pdf.
- Schmitt N. Uses and abuses of coefficient alpha. Psychological Assessment. 1996 [cited 2015 Jun 23].;8(4):350-3 Available from: http://www.psych.yorku.ca/sp/schmitt%201996_uses%20and%20abuses%20of%20coefficient%20alpha.pdf.
- Wiltshire JC, Person SD, Allison J. Exploring differences in trust in doctors among African American men and women. J Natl Med Assoc. 2011 Sep-Oct [cited 2015 Jun 11];103(9-10):845-51. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22364052.
- Lee YY, Lin JL. Trust but verify: the interactive effects of trust and autonomy preferences on health outcomes. Health Care Anal. 2009 Sep [cited 2015 Jun 11];17(3):244-60 Available from: http://www.ncbi.nlm.nih.gov/pubmed/19130247.
- Guerrero N, Mendes de Leon CF, Evans DA, Jacobs EA. Determinants of trust in health care in an older population. J Am Geriatr Soc. 2015 Mar [cited 2015 Jun 11];63(3):553-7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25752478.
