RESEARCH ARTICLE
The professionalism of clinical teachers in clinical education
Fatemeh Keshmiri, Mehran Haerizadeh, Yaser Ghelmani
Published online first on November 11, 2023. DOI:10.20529/IJME.2023.069Abstract
Background: Professionalism has long been recognised as a core competency for clinical teachers as role models and educators. The present study aimed to evaluate the adherence to professionalism of clinical teachers from the perspectives of resident doctors and undergraduate medical students.
Methods: This is a descriptive and cross-sectional study. All learners, including undergraduate medical students and residents who were studying in the medical school and teaching hospitals affiliated with Shahid Sadoughi University, were entered into this study as evaluators (n = 311). Of these, 151 clinical teachers were assessed by the learners. The students were asked to assess the two clinical teachers with whom they had interacted during the previous month in the clinical department. The Faculty Professionalism Evaluation Questionnaire was used in this study.
Results: The results of the confirmatory factor analysis (CFA) confirmed the adequacy of the model. The total mean score was 1.98 (standard deviation=0.36, range = 0.96 to 2.82). In addition, the total mean score of the adherence to professionalism among clinical teachers was reported at the level of “met expectations”. The results showed that the teachers’ scores in the domains of “doctor-patient relationship” and “doctor-student relationship” were reported under the “met expectations” level. Their scores in the “inter-professional relationship” and “doctor-self relationship” domains were reported as “below expectations”. The results showed the scores of teachers’ professionalism were significantly lower from the viewpoints of residents than in the perceptions of medical students (p=0.0001).
Conclusion: The professionalism scores of clinical teachers were evaluated as “below expectations” from the learners’ perspectives.
Keywords: professionalism, professional behaviour, clinical teacher, faculty
Introduction
Professionalism is recognised as the core competency of healthcare providers in medical education systems. Professionalism is defined as behaviours, attitudes, and manners that include adhering to ethical principles, establishing and maintaining effective communication with colleagues and patients, being trustworthy, and developing professional excellence [1, 2]. During the Covid-19 pandemic, adherence to the principles of professionalism such as compassion, altruism, respect, empathy with the patient, fairness, and managing conflicts of interest was important to improve trust between physician and patient [3]. Additionally, due to the unpredictable behaviour of the virus and the acute health condition of patients, the ability to continuously develop the professional capabilities of physicians through applying up-to-date evidence was one of the most important professional requirements in this pandemic [4, 5, 6]. The teaching of professional ethics in medicine became more complex and challenging under pandemic conditions [3, 7]. The pandemic brought out new issues in the professional domain that require urgent consideration in the healthcare system in the future.
Clinical teachers play an influential role in teaching professionalism in medical education systems and help to form learners’ professional identities [8, 9, 10, 11]. In this regard, the domain of professionalism is also considered crucial in various teacher competency frameworks [12, 13, 14, 15]. In the three-cycle model of teacher competencies, qualities such as empathy, respect for the learner, avoidance of discrimination, and respect for patient confidentiality and organisational goals were explained as features of “doing the right job” as a clinical teacher [13]. In Ali’s study, improving personal and professional abilities, helping others learn, and teamwork were introduced as three critical features of teachers’ professionalism that students observe and learn from [2]. The above-mentioned professional principles were crucial capabilities of clinical teachers as both physicians and teachers during the pandemic.
During such a crisis, clinical teachers play a prominent role in improving students’ professional capabilities such as altruism, duty, integrity, and patient confidentiality [4, 7]. Since teachers have both an explicit and an implicit effect on students’ learning [16], evaluating teachers’ professional behaviours from the perspective of learners — the most critical stakeholders of educational systems — is essential, and this was especially so during the Covid-19 pandemic. The present study was conducted to evaluate the professional behaviour of clinical teachers from the viewpoints of residents, medical interns, and medical externs during the Covid-19 pandemic.
Methods
This descriptive and cross-sectional study was conducted at Shahid Sadoughi University of Medical Sciences in Iran.
ParticipantsMedical externs were students from 3rd and 4th years of medical education (in the clerkship course), and medical interns were students from 5th and 6th years of medical education studying in the internship course. The residents were those who studied in the special education residency programme.
Inclusion criteriaThe participants had to be medical learners in undergraduate and postgraduate programmes (including medical externs, medical interns, and residents) who had spent at least three months in clinical education.
Exclusion criteriaParticipants who had less than three months since the beginning of the training course, or were in departments that did not directly interact with clinical teachers, or did not want to participate in the study, were excluded.
Validation phaseThe questionnaire’s confirmatory factor analysis (CFA) was assessed by the participating medical interns and medical externs in the medical school of a satellite campus of Shahid Sadoughi University of Medical Sciences (n=300).
Descriptive phaseAll learners (n=311) including medical externs, medical interns (undergraduate medical students), and residents (postgraduate learners) who studied in the medical school of original campus of Shahid Sadoughi University of Medical Sciences, were entered as evaluators. The medical learners evaluated 151 clinical teachers who teach in the clinical departments. The questionnaire was given to the learners with a list of clinical teachers in each department. The learners had to evaluate those clinical teachers who had interacted with them in the previous month. The teachers’ professionalism scores were calculated through the mean scores of assessments submitted by at least two learners.
Study toolA Faculty Professionalism Evaluation Questionnaire developed by Todhunter et al [17] and validated by Garshasbi et al [18] (Cronbach’s alpha = 0.88) was used in this study. This questionnaire includes four domains: doctor-patient relationship (6 items), doctor-student relationship (3 items), interprofessional relationship (2 items), and doctor-self relationship (5 items). Scores assigned were: 3 “exceeded expectations”, 2 “met expectations”, 1 “below expectations”, and 0 “not applicable” if the behaviour was either not observed or not applicable to the setting. The total sum of scores per form ranged from 16 to 48, while the total mean scores of items ranged from 0 to 3.
Phase I: validation of the tool
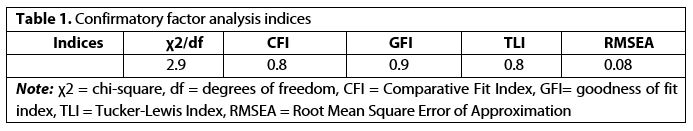
In our study, the content validity of the instrument was assessed by a panel of experts in medical education and clinical specialties (n=13). Experience in teaching and research in the professional field of at least three years was determined as inclusion criteria. After approval by the expert panel of the tool’s content validity, the CFA of the instrument was assessed by the participating medical interns and medical externs (n=300). The model parameters were estimated using the maximum likelihood method. CFA goodness-of-fit indices, including the comparative fit index (CFI), Tucker-Lewis index (TLI), and root-mean-square error of approximation (RMSEA) were calculated in order to assess the fit of the model. The model fit is acceptable based on the goodness-of-fit indices when RMSEA values of <0.08 are achieved [19, 20]. CFI values greater than 0.90 indicate a perfect fit, values between 0.80 and 0.89 represent a good but marginal fit, values between 0.60 and 0.79 indicate a poor fit, and CFI values lower than 0.60 mark an inferior fit [21]. For TLI, a value of 1 indicates a perfect model fit, while values more significant than one might indicate overfitting. TLI values lower than 0.8 indicate a poor fit [22].
Phase II: Evaluation of professionalism of clinical teachers
In the second phase, the assessment was conducted in teaching hospitals of Shahid Sadoughi University of Medical Sciences. The students evaluated the professionalism of clinical teachers who conducted clinical education courses.
Statistical analysisConfirmatory analysis was analysed using IBM SPSS Amos version 24.0 software. Data were analysed using descriptive (mean, standard deviation (SD), median, and relative percentage) and analytical tests (student’s t-test, ANOVA), and posthoc test (Bonferroni test). P value less than 0.05 was considered statistically significant.
Ethical considerationThis study was approved by the Ethics Committee at Shahid Sadoughi University of Medical Sciences (ID: IR.SSU.REC.1399.106) on May 20, 2023.
Results
Of the 311 participants, 126 (40.5%) were medical externs, 128 (41.2%) were medical interns and 57 (18.3%) residents. Of the 311 participants, 169 were male and 142 female. The mean age of participants was 26.4 (SD = 3.18) years.
The results showed that experts approved the content validity of the instrument. The results of CFA showed the adequate fitness of the model [Table 1 and Figure 1 (available online only)].

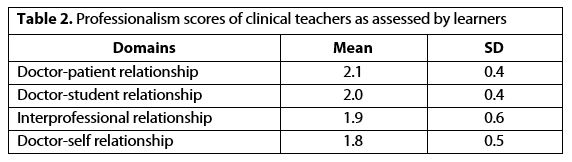
The total mean score per form as given by students was 31.91 (SD = 5.84, range = 16 to 45), with a median rating score of 32. The total mean score was 1.98 (SD = 0.36, range = 0.96 to 2.82). The professionalism scores of the clinical teachers as assessed by the participants are shown in Table 2.
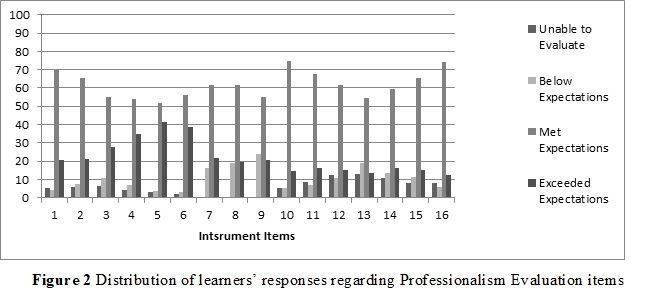
The results showed that the teachers’ scores in the doctor-patient relationship achieved the “met expectations” level. The teachers’ scores in the doctor-student relationship domain also attained the “met expectations” level. Their scores in the interprofessional relationship and doctor-self relationship domains were reported as “below expectations” level [Figure 2 and Table 2]. In addition, total mean scores for adherence to professionalism among clinical teachers were reported at the “met expectations” level.
The results showed that participants at various academic levels (p = 0.001), had differing perspectives on the professionalism scores of teachers. According to Table 3, the results showed that residents assessed the professionalism of teachers significantly lower than medical externs did (p = 0.0001). There was no difference between the scores given by residents and interns (p = 0.73), and interns and externs (p = 0.13). In the domain of the “doctor-patient relationship”, a significant difference was noted between teachers’ scores by residents and medical externs (p = 0.004) and interns (p = 0.0001). No significant difference between the teachers’ scores from the perspectives of externs and interns was reported in the “doctor-patient relationship” domain (p = 0.16). In the “doctor-self relationship” domain, teachers’ scores as assigned by residents were significantly lower than those by interns (p = 0.001) and externs (p = 0.002). Again, interns assessed teachers’ scores significantly lower than externs in this domain (p = 0.02).
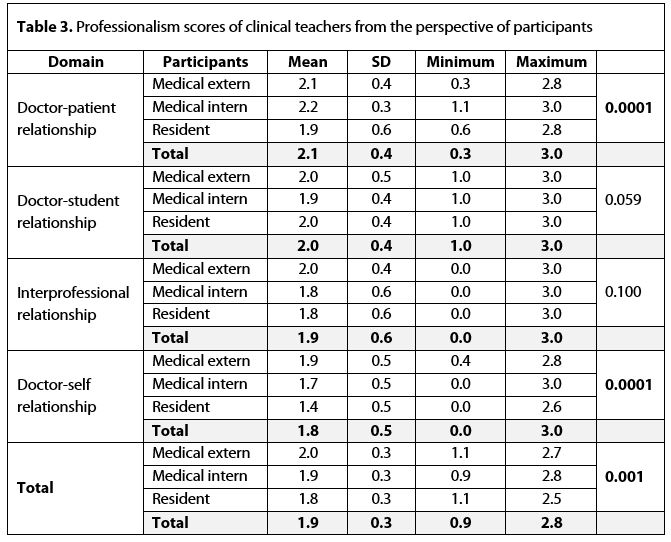
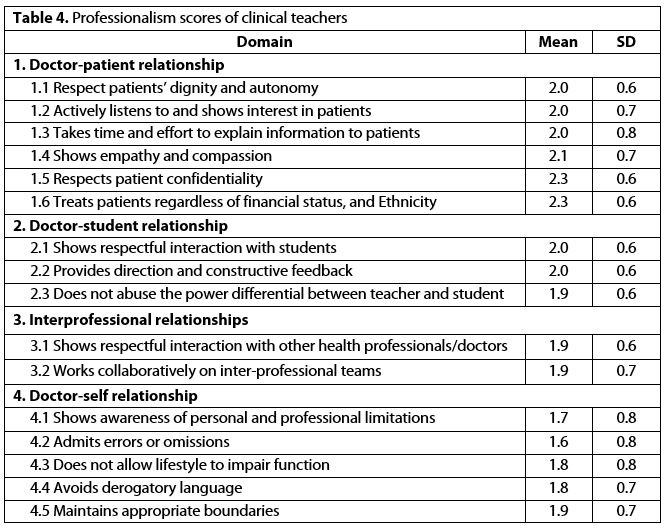
The results showed that there was no significant difference in the professionalism scores of teachers by gender of participants (p = 0.35). The mean scores of professionalism items for clinical teachers are shown in Table 4.
Discussion
During the Covid-19 pandemic, concerns about professional dilemmas and their impact on learning and forming learners’ professional identities have intensified [23]. The nature of experiential learning in the clinical education process increases the importance of professional commitment among clinical teachers as role models for students. The present study showed that professionalism scores assigned to clinical teachers by learners were below the “met expectations” level during the pandemic. Professionalism scores of clinical teachers in the domains of “doctor-patient relationship” and “doctor-student relationship” were moderate, and their scores in the domains of “interprofessional relationship” and “doctor-self relationship” were reported as “below expectations”.
The present results showed that clinical teachers obtained the highest scores in the domain of “doctor-patient relationship”, which were at the “met expectations” level. Similar to our results, the findings of earlier studies indicated that clinical teachers had a more positive attitude in terms of integrity and honesty toward patients than towards peers, collaborators, and managers [24, 25, 26, 27]. It seems that the predominantly therapeutic role of clinical teachers compared to their other roles has made teachers more sensitive in their professional commitment towards patients. In our study, the highest scores of teachers regarding professional behaviour were in observance of two principles — confidentiality and non-discrimination — towards patients, which can be effective in acquiring patients’ trust. These behaviours were critical elements in providing healthcare services to patients who fell ill with Covid-19 [3, 7]. Since the investigated hospital, as a referral center, admitted non-native patients of different religions and ethnicities, fair treatment of patients by clinical teachers can be a desirable behavioural model for learners during pandemics.
Healthcare workers were confronted with a new and unknown virus that required them to upgrade their professional capabilities continually and improve their competency to manage difficult situations arising during the pandemic [4, 7]. The lowest scores were reported in the domain of the “doctor-self relationship”, which were “below expectations”. In this domain, recognition of individual limitations, acceptance of error, balance in personal and professional life, and observance of professional principles in communication and professional performance were evaluated. The results of Garshasbi’s study confirmed the lowest scores in the domain of “doctor-self relationship” [18]. Lack of knowledge, or acceptance of the domain components as a professional principle among clinical teachers, may affect the results. The two lowest scores of items “admits errors or omissions” and “awareness of personal and professional limitations” were reported in the domain. The results indicated that learners acknowledged that the clinical teachers were not good role models in regard to these items. Armitage and Nellums identified inadequate education as one of the barriers to medical error disclosure during the pandemic [28].
Medical error disclosure and management were reported as the main issues during the pandemic [28]. Similarly, the results of Grover et al showed that residents and faculty members generally do not report their own experiences related to medical error [29]. The results that affected the teachers’ performance as inappropriate role models may have resulted from a lack of support in medical error situations, defects in error reporting and disclosure systems, and fear of punishment and inadequate laws. A flawed learning cycle, related to the management of medical errors, adversely affects the performances of learners in their careers. The positive association between the challenges posed by medical errors and the suffering from burnout and decreasing well-being of physicians [29, 30] makes it vital for learners to be trained on how to manage medical errors. Trained clinical teachers can be a good model for managing clinical errors among learners [8].
In the Covid-19 epidemic, individual challenges such as stress management, burnout, lack of self-management, and lack of emotional management, as well as professional limitations such as not recognising the need to manage difficult and stressful situations in treating patients, can have a negative impact on teachers’ clinical practice [31, 32]. Undoubtedly, weakness in the self-doctor relationship domain of clinical teachers during the pandemic can have adverse effects on the provision of health services. Recognising personal and professional abilities and limitations, having a positive attitude, and asking for assistance from colleagues and peers were considered core competencies of the professionalism of a physician [33, 34]. Our study found the poor performance of the clinical teachers in the item of “personal and professional limitation”. Menon and Padhy have identified staff burnout as one of the health system challenges in the pandemic [35]. The development of coping strategies for healthcare workers was considered a way to maintain and improve the quality of healthcare [35, 36]. During the pandemic, there was an increase in the need to establish support systems to develop professional behaviours, for the safety of personnel, especially physicians [37]. Since the fatigue or exhaustion of teachers can have a negative effect on learners, the use of counselling mechanisms and empowerment of teachers in relation to the principles of well-being and wellness was suggested, especially during this pandemic [35, 36].
During the pandemic, cooperation and teamwork were considered as the most important way to provide high-quality services. Weak interprofessional communication and teamwork challenges can have a negative impact on treatment outcomes and further staff burnout [38, 39, 40]. Respectful relationships and cooperation between different professions were evaluated in the inter-professional relationship domain. The scores of clinical teachers in this domain were evaluated as “below expectations” level in the learners’ viewpoints. These results may occur due to the non-adherence of personnel to the team-based approach in the investigated hospital. Similarly, the study findings of Garshasbi et al indicated low scores in the interprofessional relationship domain [18]. In line with our results, the findings of Aghamohammadi revealed that the lowest attitude scores of clinical teachers were reported in the domain of cooperation with physicians and nurses [24]. Despite the development of interprofessional training and collaboration in educational systems, challenges such as hierarchical relationships, doctor-centeredness, and interdisciplinary discrimination were key barriers to implementing team-based care in the investigated context [41]. The challenges and negative role models had adversely affected the development of a positive attitude towards teamwork in the future careers of learners.
The scores in the doctor-student relationship domain, which measured respectful relationships, constructive feedback, and abuse of power, were reported as being at a moderate level. The interns gave the lowest scores to their clinical teachers in this domain. The results may have been due to the negative effect of the pandemic on medical education. Besides, the low scores of teachers in this domain from the interns’ viewpoints could be due to the existence of an educational hierarchy. In the investigated educational system, increasing the number of residents resulted in a weakening of the teachers’ relationships with interns. This causes a lacuna in the process of students’ experiential learning, due to the reduction of opportunities to observe clinical teachers and receive feedback from them. In addition, ambiguity about the role of interns and lack of recognition of their role in the team can affect their understanding of the abuse of power by teachers. The results of the study by Young et al showed that respectful relationships with students were the most influential factor in evaluating the overall performance of teachers [42]. In the study by Garshasbi et al, the highest scores were related to the domain of the teacher-student relationship, which is different from the current study’s results [18]. Our results may have been influenced by the pandemic period. In that domain, the items “abuse of power” and “providing constructive feedback” were evaluated as “below expectations” in our study. Similarly, the study by Todhunter et al showed the lowest scores associated with “constructive feedback” [17]. Therefore, a clear description of the tasks of team members, creating educational situations based on a feedback-reflection process, and creating positive and structured relationships among teachers and learners are suggested.
The results of our study showed that the scores assigned by residents on teachers’ professionalism in the domains of “doctor-self relationships” and “doctor-patient relationships” were lower than those by undergraduate learners, which could be due to their having more experience and a greater awareness of a teacher’s professional performance in the educational system.
The limitations of our study were the sample size of participants and the restriction of the evaluation from the viewpoints of learners as a group of stakeholders. The use of 360-degree evaluation from the perspective of other stakeholders such as peers, and managers, as well as increasing the number of evaluations to increase reliability, is recommended.
The pandemic as a crisis period has had a negative effect on the professional behaviour of clinical teachers. In our study, the validation of the questionnaire was approved. The results of confirmatory factor analysis revealed the adequate fitness of the model in four domains. Our results indicated that clinical teachers were not ideal role models. The professionalism scores assigned to clinical teachers were below expectations, from the learners’ perspective, during the Covid-19 pandemic. The teachers’ scores in the domain of “doctor-patient relationship” were higher than in other domains. The lowest scores of teachers were reported in the domain of “doctor-self relationship” and items related to awareness of limitations and acceptance of errors. Therefore, the questionnaire could be used in the formative assessment of the professionalism of clinical teachers. Additionally, it is necessary to empower teachers and create systems providing for continuous evaluation of the development of professional behaviour among clinical teachers during crises.
Acknowledgement: We would like to thank the participants who have been involved in the study phases.
Funding: This study was funded by Shahid Sadoughi University of Medical Sciences. (ID: 5449)
References
- Wilkinson T, Wade W, Knock L. A blueprint to assess professionalism: results of a systematic review. Acad Med. 2009;84(5):551–8. https://doi.org/10.1097/ACM.0b013e31819fbaa2
- Ali A, Anakin M, Tweed MJ, Wilkinson TJ. Towards a Definition of Distinction in Professionalism. Teach Learn Med. 2020;32(2):126-38. https://doi.org/10.1080/10401334.2019.1705826
- Dhai A, Veller M, Ballot D, Mokhachane M. Pandemics, professionalism and the duty of care: Concerns from the coalface. S Afr Med J. 2020 [cited 2022 May 14];110(6):450-2. Available from: https://pubmed.ncbi.nlm.nih.gov/32880548
- Basouli M, Derakhsh S. Assessing the Need to Pay Attention to the Ethical Considerations of Medical Staff in Dealing with Patients with Covid-19. J Med Ethics Hist Med. 2021[cited 2022 Apr 11];14(1):197-215. Available from: http://ijme.tums.ac.ir/article-1-6346-en.html
- Ćurković M, Košec A, Ćurković D. Medical professionalism in times of Covid-19 pandemic: is economic logic trumping medical ethics? Intern Emerg Med. 2020 [cited 2022 Nov 5];15(8):1585-6. https://doi.org/10.1007/s11739-020-02446-5
- McQuoid-Mason D. Covid-19 and patient-doctor confidentiality. S Afr Med J. 2020 [cited 2021 Apr 24];110(6):461-2. https://pubmed.ncbi.nlm.nih.gov/32880552/
- Shi W, Jiao Y. The Covid-19 pandemic: a live class on medical professionalism. QJM. 2021:13;14(9): 677-8. https://doi.org/10.1093/qjmed/hcaa157
- Passi V, Johnson S, Peile E, Wright S, Hafferty F, Johnson N. Doctor role modelling in medical education: BEME Guide No. 27. Med Teach. 2013;35(9):1422-36. https://doi.org/10.3109/0142159x.2013.806982
- West CP, Shanafelt TD. The influence of personal and environmental factors on professionalism in medical education. BMC Med Educ. 2007 30;7(1):1-9. https://doi.org/10.1186/1472-6920-7-29
- Birden H, Glass N, Wilson I, Harrison M, Usherwood T, Nass D. Teaching professionalism in medical education: a Best Evidence Medical Education (BEME) systematic review. BEME Guide No. 25. Med Teach. 2013;35(7):e1252-e66. https://doi.org/10.3109/0142159x.2013.789132
- Barnhoorn PC, Houtlosser M, Ottenhoff-de Jonge MW, Essers GT, Numans ME, Kramer AW. A practical framework for remediating unprofessional behavior and for developing professionalism competencies and a professional identity. Med Teach. 2019;41(3):303-8. https://doi.org/10.1080/0142159x.2018.1464133
- Srinivasan M, Li S, Meyers F, Pratt D, Collins J, Braddock C, et al. “Teaching as a Competency”: Competencies for Medical Educators. Acad Med. 2011;86(10):1211-20. https://doi.org/10.1097/acm.0b013e31822c5b9a
- Hesketh E, Bagnall G, Buckley E, Friedman M, Goodall E, Harden R, et al. A framework for developing excellence as a clinical educator. Med Educ. 2001;35(6):555–64. https://doi.org/10.1046/j.1365-2923.2001.00920.x
- Cruess RL, Cruess SR. Teaching professionalism: general principles. Med Teach. 2006;28(3):205-8. https://doi.org/10.1080/01421590600643653
- Demirkasımoğlu N. Defining “Teacher Professionalism” from different perspectives. Procedia Soc Behav Sci. 2010;9:2047-51. https://doi.org/10.1016/j.sbspro.2010.12.444
- Cruess RL, Cruess SR, Boudreau JD, Snell L, Steinert Y. Reframing medical education to support professional identity formation. Acad Med. 2014;89(11):1446-51. https://doi.org/10.1097/acm.0000000000000427
- Todhunter S, Cruess SR, Cruess RL, Young M, Steinert Y. Developing and piloting a form for student assessment of faculty professionalism. Adv Health Sci Educ Theory Pract. 2011;16(2):223-38. https://doi.org/10.1007/s10459-010-9257-0
- Garshasbi S, Bahador H, Fakhraei N, Farbod A, Mohammadi M, Ahmady S, et al. Assessment of Clinical Teachers’ Professionalism in Iran: From Residents and Fellowships’ Perspective. Acta Medica Iranica.2017 [cited 2022 Nov 15];55(1):59-67.PMID: 28188945. Available from: https://acta.tums.ac.ir/index.php/acta/article/view/5786/4891
- Hooper D, Coughlan J, Mullen M. Structural equation modelling: guidelines for determining model fit. Dublin Institute of Technology ARROW@ DIT. 2008 [cited 2021 Dec 28]; 6:53–60. Available from: https://mural.maynoothuniversity.ie/6596/20
- Marsh HW, Hau K-T, Wen Z. In search of golden rules: Comment on hypothesis-testing approaches to setting cutoff values for fit indexes and dangers in overgeneralizing Hu and Bentler’s (1999) findings. Struct Equ Modeling 2004;11(3):320-41. https://doi.org/10.1207/s15328007sem1103_2
- Knight GP, Virdin LM, Ocampo KA, Roosa M. An examination of the cross‐ethnic equivalence of measures of negative life events and mental health among Hispanic and Anglo‐American children. Am J Community Psychol. 1994;22(6):767-83. https://doi.org/10.1007/BF02521558
- Bartholomew DJ, Knott M, Moustaki I. Latent variable models and factor analysis: A unified approach: John Wiley & Sons; 2011 [cited 2022 Nov 12]. https://doi.org/10.1002/9781119970583
- Sahoo S, Mehra A, Suri V, Malhotra P, Yaddanapudi N, Puri G, et al. Lived experiences of the Corona survivors (patients admitted in COVID wards): a narrative real-life documented summaries of internalized guilt, shame, stigma, anger. Asian J Psychiatr. 2020 [cited 2022 May 25];53:102187. https://doi.org/10.1016/j.ajp.2020.102187
- Aghamohammadi M, Hashemi A, Karbakhsh M, Bahadori M, Asghari F. Clinical faculty members’ attitude toward Medical Professionalism: A case study of Tehran University of Medical Sciences. Research in Med Educ. 2019 [cited 2022 May 15];11(4):13-20. Available from: http://magiran.com/p2100129
- Malekzadeh R, Amirkhanlou A, Abedi G, Araghian Mojarad F. Ethical Challenges of Care and Treatment for Patients with Covid-19 in a Hospital from the Perspective of Service Providers. J Med Ethics Hist Med 2021;14(1):140-52. https://doi.org/10.18502/jmehm.v13i24.4955
- Campbell E, Regan S, Gruen R, Ferris T, Rao S, Cleary P, et al. Professionalism in medicine: results of a national survey of physicians. Ann Intern Med. 2007;147(11):795- 802. https://doi.org/10.7326/0003-4819-147-11-200712040-00012
- Jauregui J, Gatewood M, Ilgen J, Schaninger C, Strote J. Emergency Medicine Resident Perceptions of Medical Professionalism. West J Emerg Med. 2016;17(3):355. https://doi.org/10.5811/westjem.2016.2.29102
- Armitage R, Nellums LB. Whistleblowing and patient safety during Covid-19. EClinicalMedicine. 2020;24. https://doi.org/10.1016/j.eclinm.2020.100425
- Grover A, Appelbaum N, Santen SA, Lee N, Hemphill RR, Goldberg S. Physician mistreatment in the clinical learning environment. Am J Surg. 2020. 220(2):276-281. https://doi.org/10.1016/j.amjsurg.2019.11.038
- Wallace JE, Lemaire JB, Ghali WA. Physician wellness: a missing quality indicator. Lancet. 2009;374 (9702):1714-21, https://doi.org/10.016/S0140-6736(09)61424-0
- Robert R, Kentish-Barnes N, Boyer A, Laurent A, Azoulay E, Reignier J. Ethical dilemmas due to the Covid-19 pandemic. Ann Intensive Care. 2020;10(1):1-9. https://doi.org/10.1186/s13613-020-00702-7
- Sperling D. Ethical dilemmas, perceived risk, and motivation among nurses during the Covid-19 pandemic. Nurs Ethics. 2021;28(1):9-22. https://doi.org/10.1177/0969733020956376
- Hicks PJ, Schumacher D, Guralnick S, Carraccio C, Burke AE. Domain of Competence: Personal and Professional Development. Acad Pediatr. 2014;14:S80-S97. https://doi.org/10.1016/j.acap.2013.11.017
- Tehrani SS, Nayeri F, Parsapoor A, Jafarian A, Labaf A, Mirzazadeh A, et al. Development of the first guideline for professional conduct in medical practice in Iran. Arch Iran Med. 2017 [cited 2022 May 5];20(1):12-15. PMID: 28112525. Available from: https://pubmed.ncbi.nlm.nih.gov/28112525/
- Menon V, Padhy SK. Ethical dilemmas faced by health care workers during Covid-19 pandemic: issues, implications, and suggestions. Asian J Psychiatr. 2020;51:102116-26. https://doi.org/10.1016/j.ajp.2020.102116
- Greenberg N, Docherty M, Gnanapragasam S, Wessely S. Managing mental health challenges faced by healthcare workers during Covid-19 pandemic. BMJ open. 2020: 368: 1211-21. https://doi.org/10.1136/bmj.m1211
- Perspective: the problem with the problem of professionalism. Acad Med. 2010; 85(6):1018-24. https://doi.org/10.1097/ACM.0b013e3181dbe51f
- Mohamed K, Rodríguez-Román E, Rahmani F, Zhang H, Ivanovska M, Makka SA, et al. Borderless collaboration is needed for Covid-19—A disease that knows no borders. Infect Control Hosp Epidemiol. 2020;41(10):1245-1246. https://doi.org/10.1017/ice.2020.162
- Kokudo N, Sugiyama H. Call for international cooperation and collaboration to effectively tackle the Covid-19 pandemic. Glob Health Med. 2020: 30;2(2):60-62. https://doi.org/10.35772/ghm.2020.01019
- Chakraborty C, Sharma AR, Sharma G, Bhattacharya M, Saha RP, Lee S-S. Extensive partnership, collaboration, and teamwork is required to stop the Covid-19 outbreak. Arch Med Res. 2020;51(7):728-730. https://doi.org/10.1016/j.arcmed.2020.05.021
- Vafadar Z, Vanaki Z, Ebadi A. Barriers to Implementation of Team Care and Interprofessional Education: the Viewpoints of Educational Managers of Iranian Health System. Iranian J Med Educ 2015 [cited 2022 Nov 5];14(11): 936-49. Available from: http://ijme.mui.ac.ir/article-1-3427-en.html
- Young ME, Cruess SR, Cruess RL, Steinert Y. The Professionalism Assessment of Clinical Teachers (PACT): the reliability and validity of a novel tool to evaluate professional and clinical teaching behaviors. Adv Health Sci Educ Theory Pract. 2014;19(1):99-113. https://doi.org/10.1007/s10459-013-9466-4