ARTICLE
Sensitising intern doctors to ethical issues in a doctor–patient relationship
Nilima D Shah, Ritambhara Y Mehta, Kamlesh R Dave
Published online: February 8, 2017
DOI: https://doi.org/10.20529/IJME.2017.040
Abstract
Introduction: There is a felt need in India to influence the ethical behaviour of doctors by giving students formal education in ethics in medical colleges. Since internship is the interface between learning and independent practice, it is important to sensitise intern doctors to ethical issues in a doctor–patient relationship at this stage.
Method: Small-group interactive sessions featuring case-based scenarios that depicted the principles of the code of conduct, confidentiality, autonomy, informed consent and truth-telling were conducted for 45 interns. A pre-post multiple-choice question (MCQ) test and a post-session 5-station Objective Structured Clinical Examination (OSCE) were conducted.
Results: The results revealed a 36% increase in the MCQ scores and a satisfactory performance in the OSCE. The interns fared better in the stations related to confidentiality, the code of conduct and informed consent than autonomy and truth-telling. The postintervention MCQ scores did not correlate significantly with the OSCE scores, thus highlighting the importance of independent knowledge-based and skill-based interventions. The feedback from the interns revealed that the intervention resulted in an increase in their knowledge of ethical principles and that it was likely to influence their future clinical practice. They opined that additional discussions and guidance at regular intervals would reinforce ethical practice further.
Conclusion: Interactive teaching using case-based scenarios and MCQs, followed by an OSCE, was effective in sensitising intern doctors to ethical issues in a doctor–patient relationship; however, more intensive and focused, continuous teaching should be planned for further enhancement of learning.
Introduction
There has been a rise in unethical practices by doctors. These have been brought to light by the print and electronic media, and have given rise to an atmosphere of scepticism in society. Doctors are probably no longer considered noble professionals or healers who would always do the patient good. Rather, they are service providers, and the patients the service users. This change may have come about partly because of the corrupt and unethical practices of a few doctors, resulting in a loss of trust in the doctor–patient relationship (1).
While it may be expected that the principles of ethics would either come from within or that budding doctors would imbibe the code of conduct by following role models, in reality, today’s medical students are unaware of the code of conduct and the general principles of ethics. A questionnaire based study by Arun Babu T et al in Pondicherry, southern India, revealed that there were major deficiencies in medical students’ understanding of medical ethics, especially issues pertaining to professional conduct, etiquette and ethics (2). A cross-sectional study in West Bengal, India, revealed that though medical students agreed that an awareness of ethics was important, their knowledge was deficient and there was no increase in their scores corresponding to additional years of medical education (3). Another study found that when medical students recorded the ethical issues encountered by them, the most common issues were related to ethics in medical education, professionalism, confidentiality, the doctor–patient relationship, informed consent and the doctor–peer relationship (4). Students may be either unaware of the code of conduct or the principles of ethics, or unable to translate the knowledge into actual practice.
To address these lacunae, in 2011, the Medical Council of India (MCI) released a document, “Vision 2015”, which states that all institutes should have a foundation course in ethics (5). The MCI’s document regarding regulations on graduate medical education also emphasises the importance of teaching ethics and professionalism across the entire MBBS curriculum (6). Recently, the MCI rolled out the Attitudes and Communication module, to be implemented in all medical colleges. However, as of now, only a few universities/colleges have a formal ethics curriculum, including St John’s Medical College, Bengaluru, the Rajiv Gandhi University of Health Sciences, and the Maharashtra University of Health Sciences. The model practised in St John’s Medical College involves instruction in ethics across the medical curriculum and reinforcement at the level of internship. The methods used are didactic lectures, seminars and clinical case discussions (7).
Various other methods of teaching and assessing the understanding of ethics and professionalism in the Indian context have been suggested. Those of teaching include interactive lectures, case vignettes, reflective exercises, feedback, portfolios, role models and art-based interventions, while those of assessment include multiple-choice questions, reflective/narrative portfolios, mini-clinical evaluation exercises, professionalism mini-evaluation exercises, the Objective Structured Clinical Examination (OSCE) and multi-source feedback (8).
As internship is the transition between learning and independent clinical practice, it would be an ideal time to sensitise budding doctors towards ethical practice. They should be made familiar with the principles of clinical ethics, and be able to put them into practice. As assessment drives learning, a teaching effort would be incomplete if the interns’ learning was not assessed. Against this background, as a start, we thought of sensitising interns to ethical issues in a doctor–patient relationship (code of conduct, confidentiality, autonomy, informed consent, truth-telling) by means of an interactive, scenario-based teaching session. The session was preceded and followed by an assessment with multiple choice questions (MCQs). An additional evaluation was done by OSCE thereafter. The OSCE comprises a circuit of short stations, in which an examiner examines each student on a one-to one basis while he/she interacts with either real or simulated patients. Each station has a different examiner. The students rotate through the stations, completing all of them. The OSCE has previously been found suitable for evaluating the ability of medical students and residents to address selected clinical– ethical situations (9). The OSCE, along with feedback, was planned with the dual purpose of assessing and enhancing learning.
Aims and objectives
The aims were to sensitise the interns to ethical issues in a doctor–patient relationship, using interactive teaching sessions featuring case-based scenarios; to assess their learning by MCQs and the OSCE; and to receive their feedback on the entire teaching–learning–assessment activity.
Methodology
Permission to carry out the project was obtained from the ethics committee of the institute. Twenty MCQs, which incorporated the five principles to be tested, were prepared. Ten questions were knowledge-based and 10 scenario-based, requiring the application of knowledge. Five OSCE stations, each depicting an ethical issue that was to be discussed, were prepared. These were the code of conduct, confidentiality, autonomy, informed consent and truth-telling. For each OSCE station, a resident doctor of psychiatry was given a case vignette and trained to enact the role of a patient (simulated patient). A write-up of the scenario, to be given to the intern at the time of the OSCE (OSCE instruction), was prepared. Checklists were prepared to assess whether the principles of ethics were followed during the intern’s interaction with the simulated patient. These were designed to be rated by the resident doctor (acting as a simulated patient) at each station.
In addition, the resident doctors were required to give the interns a global score out of five, on the basis of how well the situation was handled from the ethical point of view.
The MCQs and OSCE stations were reviewed and approved by three subject-experts. They were pilot-tested on a group of 13 volunteers (doctors from the psychiatry department) to ensure their feasibility, after which minor changes were made.
Every year, a batch of 150 intern doctors take turns to serve in the psychiatry department for 15 days as part of compulsory rotation. The project involved the intern doctors posted in the department of psychiatry, and was carried out in August and September 2014, in the first half of the interns’ 12-month internship period. It was a one-day intervention, conducted in two batches of 23 and 24 interns, respectively.
In the first half, a four-hour interactive session, using case scenarios, was conducted for the interns on ethical issues in a doctor–patient relationship. The resource material for these sessions included the MCI’s code of conduct document (10), the WHO Facilitator’s Guide for teaching medical ethics to undergraduate students in the South-East Asia region (11), and the Medical Ethics Manual of the World Medical Association (12). The 20-item MCQ test was administered to assess the interns’ knowledge of and attitude towards the topic before and after the intervention.
In the second half, the 5-station OSCE was implemented, with each intern having to interact with the simulated patient at each station one by one, for five minutes each. The interactions at the OSCE stations, time management and movement of the interns from one station to the next were supervised by a faculty member.
At the end of the OSCE, the interns were given group feedback on their performance. Their individual MCQ pre-test and post-test scores and the scores at each OSCE station were e-mailed to them, and specific feedback and clarifications were provided. The interns were also asked to fill up a feedback questionnaire on the teaching–learning activity. The data were analysed using Excel and the trial version of Statistical Package for Social Sciences, Version 16. The chi-square test and paired samples t-test were used as tests of significance. A p value of <0.05 was considered statistically significant.
Results
-
MCQ scores
-
OSCE scores
-
Relationship between MCQ scores and OSCE scores
-
Feedback from intern doctors
- The topic of ethical issues in a doctor–patient relationship is relevant to us.
- The content was delivered in a clear and appropriate manner.
- I am satisfied with this teaching–learning activity on the topic.
- My knowledge on the topic has increased as a result of this activity.
- My attitude towards ethical issues in a doctor–patient relationship has improved after the activity.
- This activity helped in enhancing my skills in handling ethical issues in a doctor–patient relationship.
- This activity is likely to influence my future practice in handling ethical issues in a doctor–patient relationship.
- I am satisfied with the MCQ-based assessment done on the topic.
- I was comfortable with assessment by OSCE
- I am satisfied with the assessment done by OSCE
- Interactive learning with case examples was very interesting.
- I seldom paid attention to issues like confidentiality and consent. I will be more careful now…
- Pre-assessment MCQs were a boost each time my attention was slipping.
- OSCE brought out my skills. I will be more comfortable now on in dealing with similar situations.
- Please include video demonstration of skills.
- This learning is likely to influence my future clinical practice.
- We need a platform to discuss and continue to learn the principles of ethics and related laws.
A total of 47 intern doctors (27 male and 20 female) enrolled themselves in this project and attended the interactive session on ethical issues in a doctor–patient relationship. Their MCQ scores before and after the intervention are summarised in Table 1. Their individual question-wise performance is summarised in Supplementary Table (i). The issues which were clear to most of the interns (more than 70%) before the intervention pertained to competence to give consent, telling the truth to the patient and reporting the unethical conduct of another doctor appropriately. The issues which were unclear to most of them (more than 70%) related to the doctrine of double effect, maintenance of the records of indoor patients, the principle behind an advance directive, the shift of values from paternalism to patient autonomy and the protocol for breaking bad news.
| Table 1: MCQ scores (out of 20) of intern doctors before and after intervention (n=47) | ||||
| Pre-test mean (%); SD | 10.4 (52); 2.7 | |||
| Post-test (%); SD | 17.5 (87.5); 2.2 | |||
| Gain in score (%) | 7.1 (35.5) | |||
| t-statistic | 18.57 | |||
| p value | <0.05 | |||
| SD: standard deviation | ||||
There was an increase in the scores for all questions after the intervention. The difference was statistically significant in 17 out of 20 questions. The three other questions were related to competence to give consent, exposing the unethical conduct of other doctors, and giving non-useful treatment to the patient. The interns’ concept of competence was clear even before the intervention; hence, a significant difference was not found. As for the exposure of the unethical conduct of another doctor, the number of interns who chose the option for how to report unethical conduct appropriately increased from 34 to only 36 after the intervention. The commonly held opinion was that one should talk to other doctors about it (n=9) rather than report it to the appropriate higher authority. In a question relating to a patient who insisted on getting a saline drip which was not really required, the interns chose to give a multivitamin tablet as placebo (n=10) before the intervention, and to tell her that her symptoms were imaginary (n=10) after the intervention.
Of the 47 interns enrolled, two dropped out for unknown reasons and hence, 45 participated in the OSCE. Their OSCE scores according to the checklist and the global impression were added up and graded out of 10. The average OSCE scores at the five stations are shown in Table 2. The scores of the interns at the stations of autonomy and truth-telling (breaking bad news) were lower than their performance at the other three stations.
| Table 2: Average station-wise OSCE scores of intern doctors (n=45) | ||
| Serial no. | Station (10 marks each) | Mean (SD) |
| 1 | Code of conduct | 7.95 (1.86) |
| 2 | Truth-telling | 6.20 (1.65) |
| 3 | Confidentiality | 7.95 (1.54) |
| 4 | Autonomy | 5.90 (1.30) |
| 5 | Informed consent | 7.90 (1.81) |
| SD: standard deviation | ||
Supplementary Table (ii) summarises the performance of the interns at each OSCE station, according to the checklists. The common drawbacks in the case of truth-telling (breaking bad news) were not assessing the patient’s perception/ information level (n=25), not addressing the patient’s emotions (n=25), and not leaving scope for future discussion (n=41). As for autonomy, the weak points of most interns related to explaining the illness to patients (n=34), telling them about the need for monitoring (n=22) and the importance of taking medicines (n=23), and mentioning follow-up (n=24).
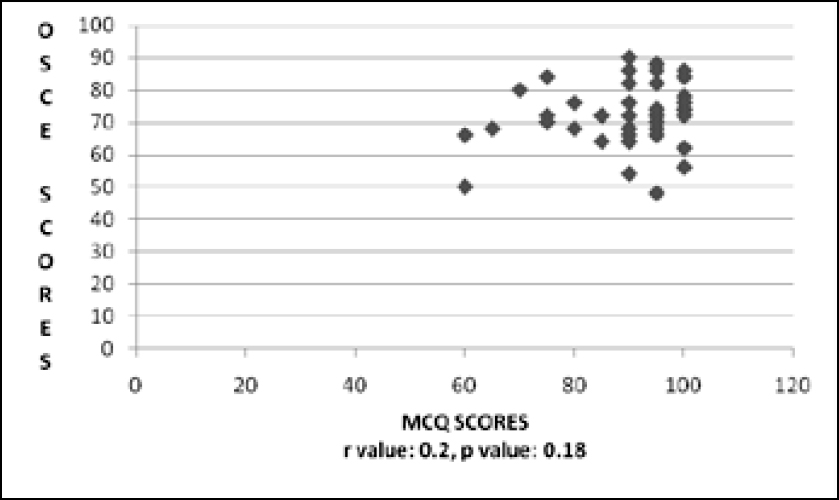
While analysing the correlation between the percentages of the post-intervention MCQ scores and the OSCE scores of the interns, a weak, non-significant correlation was found according to the Pearson’s correlation test (r=0.2, p=0.18) (Figure 1, Table 3). This means that the increase in knowledge as reflected in the MCQ scores did not correlate significantly with the improvement in performance as reflected in the OSCE.
| Table 3: Correlation between post-session MCQ and OSCE scores | |||
| MCQ | OSCE | ||
| Pearson correlation | 1 | 0.202 | |
| MCQ | Sig. (2-tailed) | 0.183 | |
| n | 45 | 45 | |
| Pearson correlation | 0.202 | 1 | |
| OSCE | Sig. (2-tailed) | 0.183 | |
| n | 45 | 45 | |
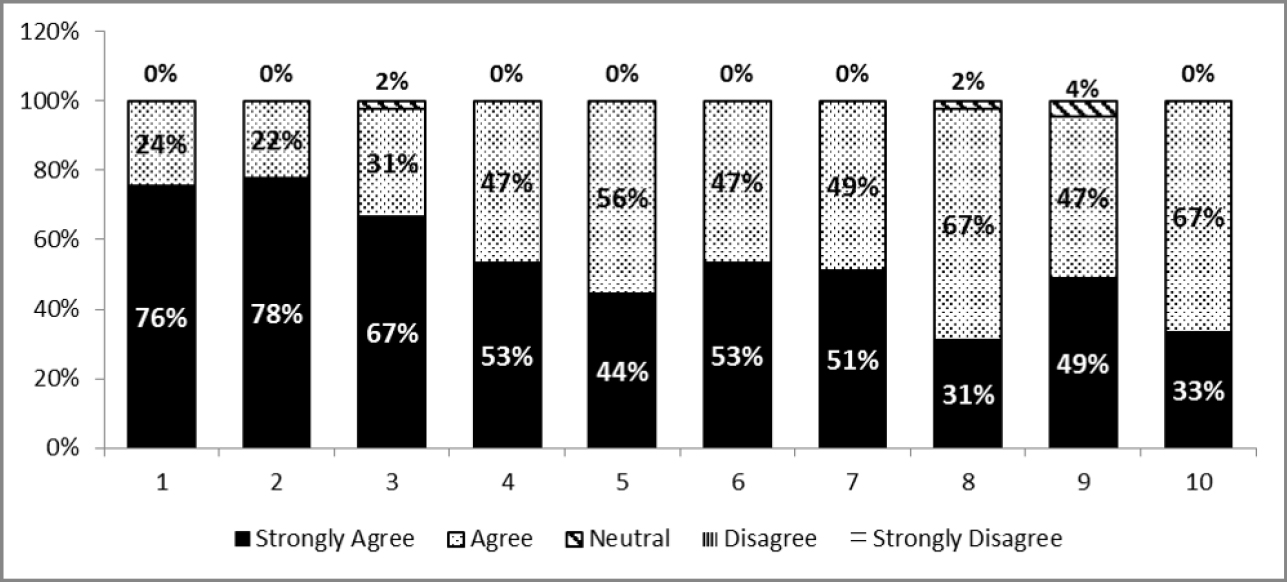
The interns’ feedback on the teaching–learning activity on a Likert scale is depicted in Figure 2. Almost all the intern doctors strongly agreed, or agreed that the topic was relevant to them, that the content was delivered in a clear manner and that they were satisfied. They strongly agreed/agreed that their knowledge, attitude and skill had improved as a result of the activity and that it was likely to influence their future practice. They also reported satisfaction with the MCQ-and OSCE-based assessment.
Opinion statements in feedback:
Some of the verbatim responses of the interns that brought out the essence of their feedback were as follows.
| Supplementary Table (i): Question-wise performance of intern doctors before and after intervention (n=47) | |||||
| Serial No. | Multiple-choice question with options | A | B | Chi square | p value |
| 1 | Which of the following was adopted by the World Medical Association as a revision of the Hippocratic Oath?
a) Declaration of Geneva b) The Helsinki declaration c) International Code of Medical Ethics d) The Nuremberg Code |
21 | 40 | 16.8574 | <0.05 |
| 2 | Therapeutic privilege means that the doctor
a) may not reveal the truth to the patient if he thinks it will cause him severe psychological harm. b) can decide which treatment is in the best interest of the patient. c) has the right to breach confidentiality if required. d) can take his professional fees for the treatment as desired. |
24 | 39 | 10.8295 | <0.05 |
| 3 | What is meant by the doctrine of double effect?
a) Giving a treatment for a desired advantage also has a simultaneous harmful effect. b) Breaching a patient’s confidentiality for public interest has the harmful effect of ruining the doctor–patient relationship. c) Preserving the patient’s autonomy may cause a disturbance in the family’s autonomy. d) Telling a patient the truth about his/her having a terminal illness may cause additional severe psychological harm. |
12 | 43 | 42.1138 | <0.05 |
| 4 | If a patient becomes incompetent to give consent, the advance directive serves to preserve the patient’s
a) autonomy. b) privacy. c) confidentiality. d) respect. |
10 | 38 | 33.3768 | <0.05 |
| 5 | As per the Medical Council of India’s Code of Conduct, the records of all indoor patients should be preserved for a minimum period of
a) 1 year. b) 3 years. c) 5 years. d) 10 years. |
9 | 43 | 49.7546 | <0.05 |
| 6 | Due to the increase in corruption, the doctor–patient relationship has witnessed a change of values from paternalism to
a) autonomy. b) patient’s rights. c) utilitarianism. d) virtue ethics. |
2 | 35 | 48.5377 | <0.05 |
| 7 | ‘SPIKES’ is a protocol for
a) breaking bad news. b) breaching confidentiality. c) obtaining written informed consent. |
10 | 47 | 61.0175 | <0.05 |
| 8 | Which one of the following is a rational approach towards ethical decision-making?
a) Virtue ethics b) Intuition c) Following role models d) Obedience |
32 | 44 | 9.8947 | <0.05 |
| 9 | We conclude that the patient is incompetent to give consent if s/he.
a) makes an irrational decision. b) is illiterate. c) is unable to understand and retain information. d) fails to make a decision which is in his/her best interest. |
46 | 47 | 1.0108 | >0.05 |
| 10 | In the case of an unattended patient, which of the following decisions can be taken by a doctor, in the patient’s best interest, without getting a magistrate’s order?
a) Withdrawal of life-sustaining nutrition and hydration b) Donation of organ/bone marrow c) Non-therapeutic sterilisation d) Conducting a high-risk cardiac surgery |
20 | 36 | 11.3083 | <0.05 |
| 11 | A 22-year-old college-going female was admitted in a hospital with an acute exacerbation of asthma. One month after her discharge, her teacher approaches you and inquires about the
student’s problem, saying that she is genuinely concerned about her. What would you do? a) Appreciate the teacher’s concern and inform her about the asthma in brief b) Request her to give an application asking for the details c) Give her a copy of the discharge card for her reference d) Tell her that you are sorry, but you cannot reveal the details |
30 | 39 | 4.4139 | <0.05 |
| 12 | A 35-year-old patient infected with HIV refuses to reveal the truth to his wife even after you have tried to convince him to do so. He says he mostly uses a condom, so it should not be a problem. What should you do?
a) Respect his confidentiality. b) Try to convince his parents to intervene in the situation. c) Tell him that you will not treat him if he does not inform his wife. d) Inform his wife. |
29 | 41 | 8.0571 | <0.05 |
| 13 | A five-year-old was admitted in hospital for high-grade fever and convulsions. He was found to be suffering from severe encephalitis and you think that he is likely to suffer from irreversible cognitive decline. How should you deal with his parents when they ask about the prognosis at the time of discharge?
a) Gently reassure them that everything will be all right. b) Wait till they realise themselves that their son is not making a full recovery, and then clarify the issue. c) Avoid telling the parents about the prognosis, but inform a distant relative. d) Inform them about the poor prognosis. |
28 | 47 | 23.8133 | <0.05 |
| 14 | A 35-year-old man has been admitted in hospital for 2 weeks with symptoms of gastric outlet obstruction. He is found to be suffering from stomach cancer and needs to be operated upon. His prognosis is poor. You are apprehensive that if you tell him this, he may not agree to the surgery. What should you do?
a) Tell him that he needs surgery for some other reason and take his consent. b) Explain the situation to his wife and take her consent. c) Just tell him that you would do what is best for him. d) Inform him about his condition and help him decide if he wants the surgery. |
35 | 45 | 8.3929 | <0.05 |
| 15 | The wife of a 28-year-old male, who has severe alcohol dependence, brings her husband to the hospital for de-addiction because his elder brother recently died of alcoholic liver disease and she is afraid the same might happen to her husband. Luckily for the patient, his liver function tests turn out to be normal. His wife requests you to scare the patient by saying that the tests indicate some danger, since only then would he agree to get admitted for treatment. What would you do?
a) Tell the patient that he has got a severe problem and needs admission for de-addiction. b) Tell the patient that the reports are slightly abnormal and this will become all right if he gets admitted and stops consuming alcohol. c) Tell him that the reports are normal, but they will definitely become abnormal if he continues to take alcohol. d) Tell his wife that she should disclose the report to the patient, in her own way. |
36 | 46 | 9.5528 | <0.05 |
| 16 | A 28-year-old lady, who is 7.5 months pregnant, is found to be suffering from lung cancer. She needs urgent chemotherapy to prolong her life. She must undergo a Caesarian section to deliver the child before the therapy can be started. She refuses to consent to the surgery because she does not want to expose the child to the risks of prematurity. She also refuses to undergo chemotherapy as it would harm her unborn child. Her husband, however, says that the child should be delivered and chemotherapy started as soon as possible. What should you do?
a) Respect the patient’s wish and give supportive care. b) Take the husband’s consent, decide on caesarean section and start chemotherapy. c) Document that the patient’s decision was emotional and irrational, so her refusal is not valid. d) Refer the matter to the ethics committee of the hospital, and then do as they say. |
19 | 34 | 9.7331 | <0.05 |
| 17 | You are a newly appointed anaesthetist in a government hospital. You notice that a senior surgeon is using outdated techniques that prolong post-operative pain and the recovery time. Also, he frequently makes crude jokes about the patient in the operation theatre. You tried talking to him about it, but he would not listen. What should you do?
a) Keep quiet about it. b) Inform his patients and suggest to them that they should complain. c) Report him to the superintendent. d) Talk about his wrongdoings to the other surgeons in the unit. |
34 | 36 | 0.2238 | >0.05 |
| 18 | You have just started your private practice and it is not running very well. You are upset because you feel that you could do good to so many patients, but they are just not coming to you. What would you do?
a) Request the general practitioners in your area to refer patients to you and give them a commission in return. b) Make a formal announcement in the press, saying that you have started a practice. Indicate your specialty and the kind of problems you can deal with. c) Make a “no cure-no payment” offer till the time your practice gets established. d) Think of ways in which you can advertise your practice. |
31 | 44 | 11.1481 | <0.05 |
| 19 | A 75-year-old male suffered from acute myocardial infarction and you saved his life. On his first follow-up visit, he brings you a gift cheque worth Rs10,000 and requests you to accept it,
considering it a blessing from him. What would you do? a) Politely refuse to accept it. b) Gracefully accept it and buy yourself a medical textbook. c) Accept it and give it to a nurse who you know is in need of money. d) Accept it and use it for the treatment of poor patients. |
31 | 45 | 13.4678 | <0.05 |
| 20 | A 33-year-old female comes to you with the complaints of generalised body ache and weakness. She reports that she has had family problems and been upset for the last few days. Her routine tests do not reveal any abnormality. She insists on getting a saline drip to feel better, since that has always worked for her. What would you do?
a) Give her the saline drip to maintain the doctor–patient relationship. b) Give her multi-vitamin tablets as placebo. c) Explain to her that she needs counselling and not the saline. d) Tell her that her symptoms are imaginary and she needs to take it easy. |
29 | 34 | 1.2033 | >0.05 |
| A B: The no. of interns who answered the question correctly before and after the intervention, respectively. The correct answer is highlighted in bold letters. | |||||
| Supplementary Table (ii): Performance of the intern doctors at the OSCE stations, as per the checklists (n=45) | |||||
| Serial No. | Ethical principle to be tested | Instruction to the simulated patient | OSCE station: scenario presented to the intern doctor | Checklist | No. of interns who did it right |
| 1 | Code of
conduct |
You are a rich businessman named Dheerubhai. You have brought an expensive watch to give your doctor, who saved you from a massive heart attack. You have to insist that he should take the gift. Start the conversation by saying, “Doctor, I have come to thank you and please accept this gift from me.” In the course of the conversation, say things like, “But you saved my life. Consider this my blessing…But this is not expensive. I will feel bad if you don’t accept it.” | You have saved the life of a rich businessman, Dheerubhai, who is here to thank you and offer you an expensive gift. Deal with the situation. | Did he/she deal with the situation gently and with patience? | 42 |
| Did he/she give the correct reason for why he/she cannot accept the gift? | 39 | ||||
| Did he/she try to ensure that the patient does not feel bad? | 25 | ||||
| Did he/she manage to deal effectively with the patient’s insistence? | 38 | ||||
| Did he/she successfully refuse? | 37 | ||||
| 2 | Truth-telling | You, Sanjay-bhai, underwent a test for HIV as a routine pre-operative test. The report reveals that you are HIV-positive and the doctor has called you to discuss the matter. Keep standing and appear nervous. | A 40-year-old male, Sanjay-bhai, who was admitted for hernia surgery, has come to see you. The routine preoperative test revealed that he is HIV-positive. He has read the report. Break the news to him. | Did he/she make the patient comfortable before he began? | 37 |
| Did he/she explore the patient’s perception/information level? | 20 | ||||
| Did he/she give the patient the basic information about HIV? | 44 | ||||
| Did he/she use simple understandable language? | 43 | ||||
| Did he/she address the patient’s emotions? (by asking/validating statements/reflecting) | 20 | ||||
| Did he/she give the patient an opportunity to ask questions? | 26 | ||||
| Was the overall conversation smooth and empathetic? | 42 | ||||
| Did he/she leave any scope for future discussion? (telling the patient about follow-up or talking about the next visit)? | 04 | ||||
| 3 | Confidentiality |
You are Siddharth. Your wife, Reena, was sent to her parents’ place as she had started behaving abnormally. You have found out which hospital she used to be treated in and you go there to get the records of her illness, so that you can file for divorce. You insist on
|
A female patient, Reena, was admitted in your
ward with an acute manic episode. Her parents were her caregivers. Now, sitting before you, is her husband, Siddharth. He feels cheated, as he did not know about the patient’s history of illness at the time of marriage. He wants to file for a divorce. He requests you to give a photocopy of Reena’s case papers. |
Did he/she refuse to give the records? | 45 |
| Did he/she resist the pressure created by the relative? | 44 | ||||
| Did he/she give the reason for refusal? | 38 | ||||
| Did he/she clarify when the details can be revealed? (It is only when the court asks for it.) | 20 | ||||
| Overall, was he/she polite? | 40 | ||||
| 4 | You, Kishorebhai, were recently diagnosed with diabetes mellitus, but you refuse to take medicines or insulin because you would rather try naturopathy and control your condition with the right diet and exercise. The doctor explains that you need medicines, but you refuse. Start the conversation by saying, “Doctor, I learnt that my sugar level is high, but I don’t want to take medicines…” | Kishorebhai has recently been diagnosed with
borderline diabetes mellitus. You believe that he should start oral hypoglycaemic medicines. However, he insists he will control his sugar with dietary measures and exercise. Deal with the situation. |
Did he/she explain in short what happens in diabetes? | 11 | |
| Did he/she explain why it is necessary to take medicines? | 23 | ||||
| Did he/she talk about the need to monitor the sugar level? | 22 | ||||
| Did he/she mention the risks of an elevated sugar level? | 43 | ||||
| Did he/she show respect for the patient’s opinion (by avoiding being rude/judgmental)? | 29 | ||||
| Did he/she mention follow-up? | 21 | ||||
| Was the overall conversation smooth
and polite? |
39 | ||||
| 5 | Informed consent | You are a 44-year-old male, Heerabhai, who suffers from hernia. You have been told that you need a surgery. Start the conversation by saying, “Doctor, what exactly is the problem with me? What is a hernia?” If given an opportunity to ask questions, ask, “Can this swelling subside with medicines?” or “Can this happen to me again after the surgery?” | Obtain written informed consent for surgery from Heerabhai, who has an inguinal hernia. | Did he/she explain the diagnosis? | 39 |
| Did he/she talk about the surgery in short? | 42 | ||||
| Did he/she speak of the risks of the surgery? | 29 | ||||
| Did he/she explain the risk of not undergoing the operation? | 32 | ||||
| Did he/she leave room for questions? | 27 | ||||
| Did he/she answer the queries adequately? | 39 | ||||
| Did he/she take written informed consent? | 39 | ||||
| Overall, was the conversation smooth and empathetic? | 42 | ||||
| Did he/she use simple, understandable language? | 35 | ||||
Discussion
There was a statistically significant increase in the interns’ knowledge of various principles of ethics, as reflected in their MCQ scores. Their knowledge regarding competence to give consent, truth-telling and exposing the unethical conduct of another doctor was good even before the intervention. They may have learnt about these matters by reading, formal and informal interaction with teachers, or observing role models during their medical curriculum.
However, most of them were not aware of the doctrine of double effect, the duration for which indoor patients’ records need to be maintained, the principle behind advance directives, shift of practice from paternalism to patient autonomy and the protocol for breaking bad news.
The scores improved for all the questions after the intervention (average increase – 35.5%), which means that while ethics is popularly believed to be only “caught”, it can also be “taught”. In the question-wise analysis, however, there was no significant difference in the question related to reporting the unethical conduct of another doctor. While the MCI states that it is the duty of every doctor to expose the unethical conduct of another (7), whistle-blowing gives rise to certain apprehensions in India. Though 34 of the 47 interns agreed to appropriate reporting of the unethical conduct of another doctor even before the intervention; only two more agreed after the intervention. The reluctance to speak out may be due to fear of being harassed, fear of disciplinary action against oneself, and fear of possible undue damage to one’s career prospects. Doctors who raise such concerns probably do not feel protected enough (13). Another opinion that did not change significantly after the intervention pertained to giving intravenous saline to a patient who actually did not need it. This probably shows a lack of awareness of somatoform illness and of the undue preference for placebo treatment in such cases. A survey of medical interns in New York revealed that those who were aware of the use of placebo would consider using it for suspected factitious pain, for patients with a history of substance abuse or psychiatric illness, or those whose complaint had a suspected psychiatric component (14). There are important ethical considerations involved in the use of intravenous saline as a placebo medication for somatoform illness. These include deceiving the patient, wasting resources and depriving the patient of the appropriate treatment. The intervention did not have any significant success in driving home these points.
The OSCE scores of the interns ranged from 5.9 to 7.95 out of 10. Their performance was significantly better in the stations related to the code of conduct, confidentiality and informed consent than autonomy and truth-telling (breaking bad news). Autonomy is a concept that dominates modern ethics. However, the minds of budding Indian doctors are perhaps still coloured by the tradition of paternalism in the doctor–patient relationship. The notion that the doctor knows what is best for the patient and the patient must comply seems to influence their belief system and practice, knowingly or unknowingly. In this context, a comparative study between Malaysia and India revealed that though the Indian doctors were aware of the concept of autonomy, the practices chosen by them reflected medical paternalism. The doctors’ opinions played a substantial role in clinical decision-making in India (15).
The interns also probably found it difficult to break bad news. This could be because the doctor may worry about how the patient would react to the bad news and handle the situation. It could also reflect the doctor’s own anxiety about breaking the news, and his/her helplessness about how to deal with the situation. A qualitative study was carried out in Mumbai, India to learn about the perspectives of interns on the communication of bad news to patients. The interns mentioned that the main obstacles in the way of communication were time constraints, language barriers, personal fears, patients’ illiteracy, crowded wards with no privacy, and lack of training (16). Thus, it seems that more focused and exclusive training is required to cultivate expertise in breaking bad news.
The poor correlation between the post-intervention MCQ scores and OSCE scores may suggest that the two tested different areas of ethical knowledge and application. It also possibly suggests that an increase in knowledge need not be parallel to an improvement in performance. It may be so because in addition to a knowledge of the various principles of ethics, one needs to have effective communication and interpersonal skills to execute the ethical principles in day-today clinical practice. This implies that any teaching–learning activity on ethics should include both knowledge-based and skill-based activities. Also, while the OSCE does measure the actual performance of interns in a given situation, it remains an artificial, standardised setting, and the real-life scenario may be quite different. The possibility remains that the interns might have performed differently if there were no time constraints, if the patients were real patients, and if there was nobody watching them. The ideal way to test ethical performance would be to have assessments based in the work-place, such as mini-clinical evaluation exercises (Mini-CEX), professionalism – mini-evaluation exercises (p-mex), reflective portfolios, and multi-source feedback.
The feedback from the interns revealed that they were satisfied with the interactive teaching, and found the group discussion based on case scenarios very interesting. The findings of a study that looked into students’ perceptions of instruction in ethics were similar. Regarding the format of teaching, the majority of students preferred lectures with break-out sessions (60%), followed by small-group discussions only (37%). Only 3% of the students preferred individual problem-solving with virtual campus support, ie no formal teaching (17). This means that a vast majority of medical students agreed to the need for formal teaching of ethics.
While the need to educate medical students on ethics has been felt, there are several difficulties in trying to achieve this goal in the Indian setting. Some of these difficulties include the absence of a compulsory course on bioethics, the lack of a uniform, need-based ethics curriculum and the extreme shortage of medical teachers trained in bioethics (18). In spite of these problems, guidelines have been proposed on designing an ethics curriculum and it has been suggested that education on ethics be incorporated in medical education across all the years, and not be restricted to a single department (19). Recently, a curriculum has been proposed for introducing ethics education into the medical curriculum in India. This includes several innovative teaching–learning and assessment methods at various levels (20). It has also been suggested that ethics should be taught as a practical subject, and the curriculum should aim at making the students aware of ethical problems and dilemmas, teaching them the mechanisms of decision-making and informing them about the existing ethical guidelines and safeguards (21).
The intern doctors who participated in this project had not been exposed to any other ethics programme in their medical curriculum, and this project was an attempt to inculcate in them the principles of ethics in a doctor–patient relationship; and it turned out to be an effective way of sensitising them. The interactive sessions with MCQs addressed the knowledge part, while the OSCE, followed by feedback, addressed the performance and enhanced the educational impact of the intervention.
However, the ideal way to impart education on ethics would be to have an ethics programme spread across the entire medical curriculum, with reinforcement at multiple levels.
Limitations
The project covered a small group of interns and can be generalised, at the most, only to the population from which it was derived.
It was only a one-time intervention in the teaching and assessment of ethics. It would have been worthwhile to find out whether the interns retained what they had learnt at the end of the internship, but such an assessment was not made because the interns were posted in various other departments and busy preparing for entrance examinations for postgraduate courses.
The OSCE was conducted immediately after the teaching–learning session. To change one’s attitudes or practices, one needs some time to understand the information, reflect, evaluate oneself and make important decisions. To facilitate this process, a continuous platform for ongoing discussion and feedback may be required. This small intervention did sensitise the interns, but it remains to be seen how, in the absence of such a system, it would influence their future clinical practice.
Competing interests and funding source: None
Any submission of very similar work: No submission has been made for publication. However, the work was presented at the 5th National Bioethics Conference at Bengaluru, in the form of a poster.
Institute where work was done: Department of Psychiatry, Government Medical College, Surat
Acknowledgements
The project was done as a part of the Foundation for Advancement in International Medical Education and Research(FAIMER) Fellowship. However, the findings and conclusions do not necessarily reflect the opinions of the organisation.
References
- Chattopadhyay S. Corruption in healthcare and medicine: why should physicians and bioethicists care and what should they do? Indian J Med Ethics. 2013 Jul-Sep;10(3):153-9.
- Arun Babu T, Venkatesh C, Sharmila V. Are tomorrow’s doctors aware of the code of medical ethics? Indian J Med Ethics. 2013 Jul-Sep;10(3):192-4.
- Chatterjee B, Sarkar J. Awareness of medical ethics among undergraduates in a West Bengal Medical College. Indian J Med Ethics. 2012 Apr-Jun;9(2):93-100.
- Fard NN, Asghari F, Mirzazadeh A. Ethical issues confronted by medical students during clinical rotations. Med Educ. 2010 Jul;44(7):723-30.
- Medical Council of India. Vision 2015. New Delhi, March 2011 [cited 2015 Oct 14]. Available from: http://www.mciindia.org/tools/announcement/MCI_booklet.pdf
- Medical Council of India. Regulations on Graduate Medical Education, 1997 [cited 2016 Oct 27]. Available from: http://www.mciindia.org/Rulesand-Regulations/GMEREGULATIONS.pdf
- Ravindran GD, Kalam T, Lewin S, Pais P. Teaching medical ethics: a model. Issues Med Ethics. 1998 Jul-Sep;6(3):83-4.
- Modi JN, Anshu, Gupta P, Singh T. Teaching and assessing professionalism in the Indian context. Indian Pediatr. 2014 Nov;51(11):881-8.
- Singer PA, Cohen R, Robb A, Rothman A. The ethics objective structured clinical examination. J Gen Intern Med. 1993 Jan;8(1):23-8.
- Medical Council of India. Code of Ethics Regulations, 2002 [cited 2015 Oct 14]. Available from: http://www.mciindia.org/RulesandRegulations/CodeofMedicalEthicsRegulations2002.aspx
- World Health Organization. Facilitators’ guide for teaching medical ethics to undergraduates in the South-East Asia region. New Delhi: Regional Office for South East Asia; 2010 [cited 2015 Oct 14]. Available from: http://www.mcn-whosear.net/pdf/SEA-HSD-330_2010_Facilitators.pdf
- World Medical Association. Medical ethics manual, 2nd edition; 2009 [cited 2015 Oct 14]. Available from: http://www.wma.net/en/30publications/30ethicsmanual/pdf/ethics_manual_en.pdf
- Chatterjee P. Whistleblowing in India: what protections can doctors who raise concerns expect? BMJ. 2015 Feb; 350:h763.doi: 10.1136/bmj.h763.
- Berger JT. Placebo medication use in patient care: a survey of medical interns. West J Med. 1999 Feb;170(2):93-6.
- Yousuf RM, Fauzi AR, How SH, Rasool AG, Rehana K. Awareness, knowledge and attitude toward informed consent among doctors in two different cultures in Asia: a cross-sectional comparative study in Malaysia and Kashmir, India. Singapore Med J. 2007 Jun;48(6):559-65.
- Supe AN. Interns’ perspectives about communicating bad news to patients: a qualitative study. Educ Health (Abingdon). 2011 Dec;24 (3):541.
- Johnston C, Haughton P. Medical students’ perceptions of their ethics teaching. J Med Ethics. 2007;33:418-22.
- Ravindran GD. Medical ethics education in India. Indian J Med Ethics. 2008 Jan-Mar;5(1):18-19.
- Anshu. Inclusion of ethics matters in the undergraduate medical curriculum. Indian J Med Ethics. 2011 Jul-Sep;8(3):135-8.
- Mahajan R, Aruldhas BW, Sharma M, Badyal DK, Singh T. Professionalism and ethics: a proposed curriculum for undergraduates. Int J Appl Basic Med Res. 2016 Jul-Sep;6(3):157-63.doi: 10.4103/2229-516X.186963.
- Johnson AG. Teaching medical ethics as a practical subject: observations from experience. J Med Ethics. 1983 Mar;9(1):5-7.