THEME – ETHICAL AND LEGAL CHALLENGES OF VACCINES AND VACCINATION
Public trust in vaccination: an analytical framework
Vijayaprasad Gopichandran
DOI: https://doi.org/10.20529/IJME.2017.024
Abstract
While vaccination is one of the most successful public health interventions, there has always been a parallel movement against vaccines. Apart from scientific factors, the uptake of vaccinations is influenced by historical, political, sociocultural and economic factors. In India, the health system is struggling with logistical weaknesses in taking vaccination to the remotest corners; while on the other hand, some people in places where vaccination is available resist it. Unwillingness to be vaccinated is a growing problem in the developed world. This trend is gradually emerging in several parts of India as well. Other factors, such as heightened awareness of the profit motives of the vaccine industry, conflicts of interest among policy-makers, and social, cultural and religious considerations have eroded the people’s trust in vaccination. This paper develops an analytical framework to assess trust in vaccination. The framework considers trust in vaccination from four perspectives – trust in the health system, the vaccine policy, vaccination providers and specific vaccines. The framework considers specific issues involved in vaccination trust, including the increasing scepticism towards medical technology, perceptions of conflicts of interest in the vaccine policy, and of lack of transparency and openness, the presence of strong alternative schools of thought, influence of the social media. The paper will conclude by arguing that engaging with communities and having a dialogue about the vaccination policy is an ethical imperative.
Introduction
Vaccination is one of the most successful public health interventions globally. The eradication of small pox and more recently, the concerted efforts to eliminate polio provide evidence of the success of vaccination programmes (1, 2).It has been globally recognised that vaccination is an essential public health service in all nations (3). High coverage of vaccination against specific infectious diseases is required for the control of these infections (4) and 2. When the coverage is high, not only does it protect the vaccinated, but also provides herd immunity and interrupts the transmission of the infectious agent in the community.
The protection offered by the vaccination programme is influenced by the vaccination policy of a country. The policy sets out the types of vaccines to be included, the number of doses and the timing of the administration of the doses (5). The coverage of vaccination in the population depends on the availability of the vaccine, its accessibility, and the delivery of the vaccine in an effective manner. All these are functions of the health system. The key functionaries in the vaccination process are the healthcare providers, including physicians, nurses and community health workers, who administer the vaccines at the point of care. They have a strong influence on the success of the vaccination programme. At the next level are the people, who are the ultimate consumers of the vaccination programme; and their acceptance plays a vital role in the success of the programme.
While the public health system in India is grappling with issues concerning the supply side of the vaccination programme so as to be able to ensure the availability and accessibility of effective and safe vaccines to large numbers of people, there are important issues concerning the demand side which also need to be considered. In certain areas of the country, despite having easy access to vaccines, parents are hesitating to follow even the routine immunisation schedule for their children. Vaccine hesitancy is an emerging problem in the developed world and is gradually catching up in certain regions of India (6, 7, 8, 9). According to the estimates of vaccination coverage, as per the 2015–16 National Family Health Survey (NFHS-4), full immunisation coverage among children between 12 and 23 months of age was about 60% (10). Though exact data on the proportion of refusals were not available, a UNICEF estimate from a sample survey shows that refusals contributed to almost one-third of the uncovered proportion in Bihar (11). There are scarce data on the proportion of refusals in the various states and this estimate from Bihar may not be representative of the rest of the country. However, the problem of vaccine hesitancy does exist at different levels in different parts of the country. It is in this context that we need to gain an understanding of the community’s perceptions of, attitude towards and trust in vaccination.
This article will specifically explore the state of people’s confidence and hesitancy with regard to vaccination from the perspective of trust. It will develop an analytical framework which will take into account the people’s trust in the vaccination policy, and in health system, vaccination providers and specific vaccines. The framework will deal with specific issues relating to trust in vaccinations, including the increasing scepticism towards medical technology, perceptions of conflicts of interest in the vaccine policy, the availability of strong alternative schools of thought, the influence of the social media, misinformation regarding vaccinations, and the lack of transparency and openness. Finally, the article will highlight the ethical imperative to engage with communities to foster a dialogue about vaccinations to help them make informed decisions.
The vaccine decision-making model
Several decision-making models have been proposed for parents’ decisions on vaccination. The health belief model, originally proposed to assess the uptake of polio vaccination in the USA, considers perceived susceptibility to the disease, severity of the disease if it occurs, perceived benefits of and, barriers to the vaccine, and cues to action (12). Sturm et al proposed a decision-making model in which institutional, personal/parental and sociocultural/environmental influences interface with the healthcare provider and shape parental decisions (13).
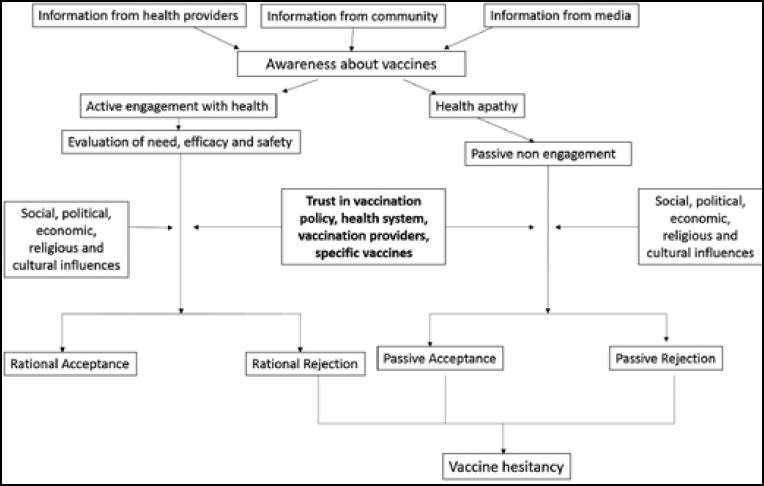
Decision-making regarding vaccination, especially in developing countries such as India, is very complex (14). Figure 1 shows a proposed decision-making model that requires empirical testing. Parents are provided information on vaccination by various sources, the most common being healthcare providers (15). This information is supplemented by information based on the experience of community members and by the media. It must be noted that all this information is not authoritative and credible. Most often, the only source of credible information, ie healthcare providers, provide inadequate information. The social media has become a powerful source of information in several urban areas and among the educated class (16). Among the less educated and rural populations, rumours are a potential source of information. All these sources create awareness (sometimes wrongly!) of vaccination. Educated and motivated people actively engage in their own healthcare, and evaluate the need for specific vaccines and their efficacy and safety (17). They access the relevant information through the Internet and social media and appraise it. However, the large rural population, whose educational attainment and health literacy levels are poorer, is not actively involved in healthcare decisions and shows passive conformism based on popular practices and trends. These people make certain decisions on vaccination because their healthcare providers have given them an “immunisation schedule card” and asked them to follow it, or because everybody else in the community does so. In certain underdeveloped areas, coercion and force are used to get people vaccinated. These people cannot really be said to make an informed vaccination choice. Among both these groups of people, several social, political, economic, religious and cultural influences play a role in determining the acceptance of vaccines (8). These include the social norm regarding vaccination, religious beliefs, historical anecdotes such as stories about vaccine failure and adverse events of vaccines, community experiences of adverse events, the cost of vaccines, perceptions of conflicts of interest among the vaccine industry and policy-makers, and the strong anti-vaccination propaganda (18). Together with these influences, trust plays a very important role in decision-making on vaccines (19). Trust, too, is influenced by sociocultural and political factors. On the one hand, there are those who accept vaccines rationally, on the basis of active engagement with the vaccination system. On the other hand, there are people who are at various stages of vaccine hesitancy, ranging from total rational rejection, partial rejection of specific vaccines, passive conformism and passive misinformed rejection. Against this background, it is important to explore the concept of trust in vaccination.
Trust in vaccination
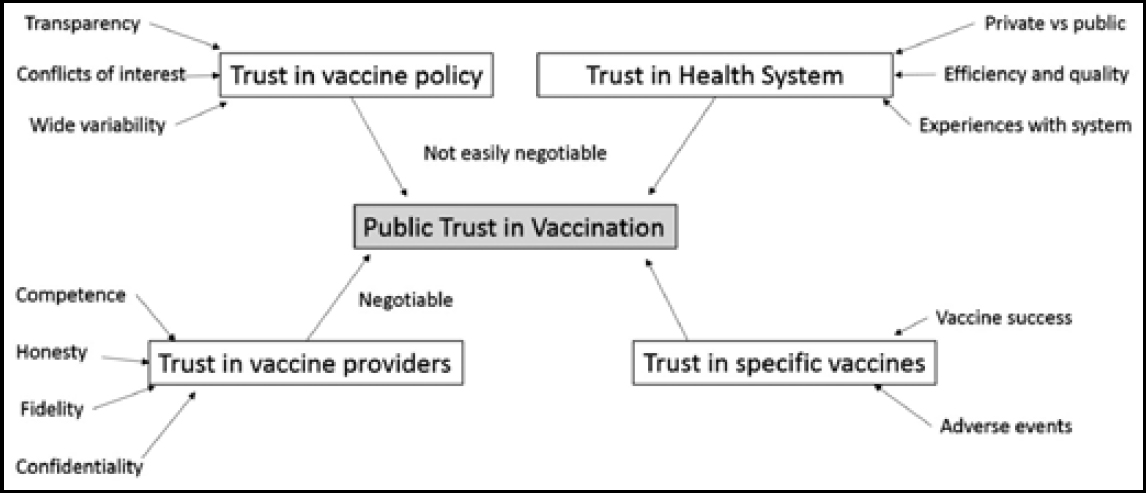
Trust is the optimistic acceptance by people of their vulnerability in the belief that the trusted party will do whatever is in their best interest (20). Trust is inherent in healthcare and is an essential component of any healthcare relationship. In the context of vaccination, trust is not a phenomenon that involves just an interpersonal relationship. People’s decision to accept vaccination depends on the trust they have at various levels of the vaccination programme, namely, policy, the health system, healthcare providers and specific vaccines (21, 22).
A trustworthy policy on vaccination is one which is transparent, engages with the communities and is open to dialogue. Before introducing a new vaccine, modifying the schedule, or changing the route or mode of administration, policymakers should engage with the communities and discuss the potential implications of such a change. This is essential to engender trust in the vaccination policy. Different countries have different vaccination schedules, as do different states within a country. This creates confusion and doubt in the minds of discerning decision-makers. In India, the policies of the public health system and the recommendations of the Indian Association of Paediatrics with respect to several childhood vaccines are competing and often conflicting (23). This conflict causes further confusion regarding the vaccination policy and leads to the erosion of trust.
Trust in the health system involves perceptions of the quality, competence, fairness and openness of the system (24, 25). India has a thriving private healthcare system and a large, but rather weak, public system. While the level of trust in the public system may be low because of the perception that it lacks competence and quality, there may be doubts about the private system because of the profit motives and conflicts of interest involved (26). In 2014, a major sting operation by a private television news channel revealed that commissions, cut practice, kickbacks and such corrupt practices were rampant among private medical practitioners in New Delhi (27). This is only one example of why trust in the private sector has given way to scepticism in recent times (28). There are innumerable examples of the steady evolution of trust from blind faith in the health system to a questioning scepticism over the past three decades. The introduction in 1986 of the Consumer Protection Act, which covers medical care as well, is an indicator of the need for legal oversight of a system with diminishing values, a system which was blindly trusted for its virtues until then. Though a vast majority of people in India still seek private healthcare for their needs, the level of trust in the private sector per se has decreased substantially (29). There is a delicate balance between the perception of competence and fidelity of the private health system when it comes to trust in the system. While it is perceived that the level of competence of the sector is high, the level of fidelity is perceived to be poor, and this is the reason for the erosion of trust. The same dynamics of trust applies when it comes to the delivery of vaccines through the public and private health systems. In several parts of India, people trust the public health system more than the private one when it comes to vaccination because the latter is suspected to be driven by profit motives. Trust in the health policy and health systems is institutional in nature and, therefore, difficult to negotiate through interpersonal interactions (30). This is in contrast to the interpersonal trust that people have in vaccination providers.
The level of trust in vaccination providers is reflected in the people’s perceptions of their competence, honesty, fidelity and confidentiality (31).The trust people have in their healthcare providers strongly influences their trust in vaccination since healthcare providers are the primary source of information on vaccinations for most people. The overriding factors determining trust in vaccination are those of efficacy and safety. Vaccines carry with them reputations that are based on reports of successful prevention of diseases and adverse events following immunisation (AEFIs). AEFIs lead to the erosion of trust in the specific vaccine. Given that no vaccine is completely free of adverse events, the vaccination policy should feature a sound surveillance system to detect AEFIs, and make provision for timely intervention and mitigation of the consequences. Following the introduction of the pentavalent vaccine in Tamil Nadu and Kerala in 2011, several vaccinated children were reported to have died. After 14 deaths were reported, investigations into the AEFIs were carried out. It was found that six deaths were due to comorbid conditions, none of which was a substantial reason to attribute the deaths to the pentavalent vaccine. A detailed analysis of the deaths also revealed that a diagnosis of sudden infant death syndrome (SIDS) was highly unlikely. The callous attitude towards investigation, reporting, response and compensation for children who had suffered fatal AEFIs led to gross erosion of trust (32). The analytical framework of public trust in vaccination, specifically on the vaccine policy, health system, vaccination providers and specific vaccines is shown in Figure 2.
It is important to note that high vaccination coverage does not necessarily reflect trust in vaccination. There are situations in which the community is not engaged in decision-making, and trust may not be said to exist but there is passive acceptance of vaccination, and also, situations in which there is a high level of trust but poor coverage due to a lack of access.
Factors leading to mistrust in vaccination
Having reflected on the role of trust in vaccination in the decision-making process and the framework of trust in vaccination, it is important to address specific issues pertaining to mistrust in vaccination.
Increasing scepticism towards science and technology
In recent years, people have started to actively engage with the world of science. In the past, when people opposed science, they were called superstitious and were looked down upon. Today, however, it is common for people to be sceptical about science and question it, which indicates greater active engagement with current developments (33). This scepticism about science emerges from three important sources: (i) an inherent difficulty in dissociating beliefs from facts, (ii) an increasingly “post-truth” policy environment, and (iii) suspicions about the way evidence is generated. Often, technological advances in healthcare give rise to interventions which are difficult to believe and follow . When long-held notions of health and disease are challenged, it becomes more difficult to dissociate facts from beliefs. Even when rational thinkers accept scientific facts, they cling to intuitions which are shaped by beliefs. This results in a delay in the adoption of scientific advancements (34).The “post-truth” policy environment, in which objective facts and evidence are usually assigned less importance than “opinions”, “beliefs” and “emotional sentiments”, has led to an increase in scepticism towards science (35). Finally, the way scientific evidence is generated has also been questioned thoroughly. The landmark paper by Ioannides in 2005 highlighted this aspect by declaring that most published research findings are false. He raised fundamental questions regarding study designs and statistical power, and concluded that most scientific research findings may simply be accurate measures of existing biases (36). The existence of financial and other conflicts of interest and research malpractices adds fuel to this suspicious approach to science, painting a negative picture of the actual practice of scientific research (37). Therefore, public health interventions are being questioned increasingly, especially when the intervention is a preventive one, such as vaccination of healthy children. Moreover, success of vaccination itself poses a threat to continued vaccination as the reduction in the incidence of the infection, reduces the perceived threat among the people (38). Parents would rather not see their children suffer from adverse events following vaccination than prevent a disease which is not common and is only a hidden threat. To sum up, the perceived threat from diseases has decreased and the scepticism regarding vaccines has grown.
Availability of strong alternative schools of thought
In several sections of Indian society, especially the upper class, there is a move towards “natural measures for health”. These include avoidance of processed foods, the promotion of herbal foods, medicines and toiletry products, and avoidance of chemicals, including medications. In these circles, vaccines are viewed as “artificial” and are looked down upon. This, along with the anti-vaccination lobby, as well as the popularity of complementary and alternative systems of medicine such as naturopathy, which oppose vaccination, has made a large contribution to the deficit of trust in vaccination (39).
Misinformation regarding vaccination
With the advances in information and communications technology, not only is information readily available to people, but it is also hidden within a huge amount of misinformation. Misinformation about vaccination spreads as fast as, or sometimes faster than, credible information. In certain districts of Uttar Pradesh and Bihar, there was serious resistance to the polio vaccination due to widespread misinformation among the minority communities that it was a western ploy to sterilise the minority populations and thus reduce their numbers (40). A deeper analysis of the social reasons for resistance to the polio vaccine in Uttar Pradesh revealed that other than the “misinformation” factor, the community was tired of the repeated rounds of the pulse polio campaign, which had led to suspicions, and the minority community was even less amenable to vaccination because the complete apathy of the mainstream health system towards their other healthcare needs had left them feeling marginalised and oppressed. The historical experiences of the minority communities with respect to the state led to widespread dissatisfaction with the health system, and this only reinforced the negative attitudes resulting from misinformation (41). This highlights how trust in vaccination is strongly influenced by trust in the health system and the social, historical and political context. Similarly, widespread misinformation regarding the introduction of a sterilising agent in the routine tetanus vaccine led to a sharp fall in the coverage of the vaccine in the Philippines (42). More recently, the coverage of the diphtheria vaccine fell drastically in the Malappuram district of Kerala following widespread misinformation on the occurrence of serious adverse events with the vaccine. This information spread more rapidly among fathers working in the Middle Eastern countries and this, in turn, reduced the vaccination rates of their children back home. The result was a serious outbreak of diphtheria in this district (43).
Influence of Internet and social media
The ease of access to information through the Internet has significantly influenced decision-making on vaccination, especially among those who are actively involved in their own and their children’s healthcare decisions. Adverse events following immunisation are no longer the subject of isolated newspaper stories that one reads, empathising with the victims. They are discussed in personalised narratives on blogs, social media platforms and virtual networks. They appeal strongly to the emotions of the audience and influence its trust in the vaccination process (44). The hugely notorious reports of an association between the Measles, Mumps and Rubella (MMR) vaccine and autism in the UK created a frenzy in the mainstream and social media, and led to an erosion of trust in the vaccination system in the country (45). In a study of anti-vaccination Twitter feeds in the USA, it was found that the people who took strong anti-vaccination stands were those who had a strong distrust of the government and were conspiracy thinkers. Those who had newly adopted an antivaccination stand, as traced from the Twitter feeds, were more social and actively questioned their beliefs (16).
Perception of conflicts of interest in vaccine policy
Doubts have been mounting about the intentions and motivations of the pharmaceutical industry. This holds good for the vaccine industry as well. The growing list of vaccines that are included in the vaccination schedule on the recommendation of private associations of doctors has given rise to concerns about the existence of a nexus between the industry and such professional bodies and policy-makers. A popular daily newspaper in India carried an item which discussed the existence of substantial conflicts of interest in the vaccination policy recommended by the Indian Association of Paediatrics Committee on Immunisation (IAPCOI). Of the IAPCOI’s fund of Rs 27.8 lakh, Rs 26.8 lakh was contributed by vaccine manufacturers, including Sanofi Pasteur, GSK, Merck, Pfizer and the Serum Institute of India (46). However, the IAPCOI denied the existence of any conflicts of interest. When the popular press carries such information, it substantially influences the people’s trust in the vaccination policy.
Lack of transparency and openness
Several adolescent girls died during the study of the human papilloma virus vaccine, conducted in Andhra Pradesh and Gujarat by PATH and the Indian Council of Medical Research. The study raised a controversy, and one of the important reasons for the erosion of trust in the vaccination system was the lack of transparency. The government stalled all efforts by civil society organisations to obtain the details of the study protocol. The government also failed to engage with the press or any form of media to explain these deaths. It was a detailed investigation by a civil society organisation that uncovered the malpractices and the details of the trial (47). Lack of transparency in the vaccination policy seriously hampers trust, and this influences the decisions of the parents.
Ethical imperative to engage with communities on vaccination
Active community engagement is one of the key measures for ensuring that the vaccination policy and health system are viewed as trustworthy (48). As mentioned earlier, trust in the vaccine provider, doctor, nurse or community health worker can be negotiated through active dialogue. However, it is difficult to build and sustain trust in the case of institutions such as the health system, since these are distant from the people; unless there specific measures are taken to promote engagement with the community. Trust is a double-edged sword. Too much trust, ie blind and unquestioning trust, can push people into a vulnerable position, while too little trust can keep them from participating in and reaping the benefits of public health interventions. To empower people with the right type and amount of trust, it is an ethical imperative to engage in a dialogue with the community (49). Active community engagement with respect to vaccination policies can comprise of the following:
- having community representatives (parents of children in the relevant age group) in vaccination committees to hear their opinions and engage them in policy decisions
- establishing a horizontal dialogue with communities during the introduction of new vaccines, change in the vaccination schedule, trials of experimental vaccines, etc., and not just focusing on the provision of information
- establishing community-based vaccination surveillance, in which data on the incidence of vaccine-preventable diseases, vaccination coverage and adverse events following vaccination are collected and reported by community members
- responsible engagement of community champions who spearhead the movement for the dissemination of credible, authoritative information on vaccines
- adopting a judicious approach to informing the community about adverse events following vaccination, so that panic is not created and at the same time, appropriate information is disseminated, ensuring transparency
- establishing appropriate mechanisms of accountability with the participation of the community members, who should be empowered to question vaccination practices and make informed decisions for themselves
- creating community ownership of the health of the children and their own future, and empowering communities to demand vaccination services and not act as just passive recipients of vaccinations
Active engagement of the community will assist those who make active and participative decisions on vaccination to be better informed. The objective of appropriate community engagement is not just to increase the acceptance of vaccines, but to promote a sense of self-determination that would allow the community members to make well-informed decisions on which vaccines to accept and reject for their children. To sum up, community engagement is an ethical imperative to help people realise their right to good health.
Conflicts of interest: The author declares no conflicts of interest.
References
- Belongia EA, Naleway AL. Smallpox vaccine: the good, the bad, and the ugly. Clin Med Res. [Internet]. 2003 [cited 2017 Feb 28];1(2):87-92. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC1069029
- Sutter RW, Maher C. Mass vaccination campaigns for polio eradication: an essential strategy for success. Curr Top Microbiol Immunol. 2006; 304:195-220.
- National V accine Advisory Committee. Protecting the public’s health: critical functions of the Section 317 Immunization Program-a report of the National Vaccine Advisory Committee. Public Health Rep [Internet]. 2013 [cited 2017 Feb 28];128(2):78-95. Available from: https://www.ncbi.nlm.nih.gov/pubmed/23450872
- Plans-Rubio P. The vaccination coverage required to establish herd immunity against influenza viruses. Prev Med. 2012;55(1):72-7. doi: 10.1016/j.ypmed.2012.02.015. Epub 2012 Mar 4.
- World Health Organization Regional Office for South-East Asia. Report of the South-East Asia Regional Vaccine Prioritization Workshop. WHO 2009:11-13.
- MacDonald NE; SAGE Working Group on V accine Hesitancy. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161-4. doi: 10.1016/j.vaccine.2015.04.036. Epub 2015 Apr 17.
- Dubé E, Laberge C, Guay M, Bramadat P, Roy R, Bettinger J. Vaccine hesitancy: an overview. Hum Vaccin Immunother. 2013;9(8):1763-73. doi: 10.4161/hv.24657. Epub 2013 Apr 12.
- Butler R, MacDonald NE; SAGE Working Group on V accine Hesitancy. Diagnosing the determinants of vaccine hesitancy in specific subgroups: the guide to Tailoring Immunization Programmes (TIP). Vaccine. 2015;33(34):4176-9. doi: 10.1016/j.vaccine.2015.04.038. Epub 2015 Apr 18.
- Velan B. Vaccine hesitancy as self-determination: an Israeli perspective. Isr J Health Policy Res. 2016 Apr 4 [cited 2017 Feb 28]; 5:13. doi: 10.1186/s13584-016-0071-x.eCollection 2016. Available from: http://dx.doi.org/10.1186/s13584-016-0071-x
- International Institute of Population Sciences. NFHS-4 FACT SHEETS FOR KEY INDICATORS BASED ON FINAL DATA [Internet]. IIPS 2016 [cited 2017 Feb 28]. Available from: http://rchiips.org/nfhs/factsheet_NFHS-4.shtml
- WHO/UNICEF. Missed children and refusal rates in Bihar [Internet]. UNICEF 2008 [cited 2017 Feb 28]. Available from: https://www.unicef.org/immunization/index_43911.html
- Janz NK, Becker MH. The Health Belief Model: a decade later. Health Educ Q. 1984 Spring;11(1):1-47.
- Sturm LA, Mays RM, Zimet GD. Parental beliefs and decision making about child and adolescent immunization: from polio to sexually transmitted infections. J Dev Behav Pediatr. 2005 Dec;26(6):441-52.
- Larson HJ, Schulz WS, Tucker JD, Smith DMD. Measuring vaccine confidence: introducing a global vaccine confidence index. PLoS Curr. 2015 Feb 25;7. pii: ecurrents.outbreaks.ce0f6177bc97332602a8e3fe7d7f7cc4. doi: 10.1371/currents.outbreaks.ce0f6177bc97332602a8e3fe7d7f7cc4.
- Jones AM, Omer SB, Bednarczyk RA, Halsey NA, Moulton LH, Salmon DA. Parents’ source of vaccine information and impact on vaccine attitudes, beliefs, and nonmedical exemptions. Adv Prev Med. 2012 [cited 2017 Feb 28]; 2012:932741. doi: 10.1155/2012/932741. Published online 2012 Oct 2. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3469070&tool=pmcentrez&rendertype=abstract
- Salathé M, Khandelwal S. Assessing vaccination sentiments with online social media: implications for infectious disease dynamics and control. PLoS Comput Biol. 2011 Oct;7(10):e1002199. doi: 10.1371/journal.pcbi.1002199. Epub 2011 Oct 13.
- Greenhalgh T, Wessely S. “Health for me”: a sociocultural analysis of healthism in the middle classes. Br Med Bull. 2004; 69:197-213.
- Kumar D, Chandra R, Mathur M, Samdariya S, Kapoor N. Vaccine hesitancy: understanding better to address better. Isr J Health Policy Res. 2016 Feb 1 [cited 2017 Feb 28]; 5:2. doi: 10.1186/s13584-016-0062-y. Published online 2016 Feb 1. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=4736490&tool=pmcentrez&rendertype=abstract
- Larson HJ, Cooper LZ, Eskola J, Katz SL, Ratzan S. Addressing the vaccine confidence gap. Lancet. 2011 Aug 6;378(9790):526-35. doi: 10.1016/ S0140-6736(11)60678-8.
- Hall MA, Dugan E, Zheng B, Mishra AK. Trust in physicians and medical institutions: what is it, can it be measured, and does it matter? Milbank Q. 2001;79(4):613-39, v.
- Schwartz JL. Unintented Consequences: the primacy of public trust in vaccination. Mich L Rev First Impressions. 2009 [cited 2017 Feb 28]; 107:100-4. Available from: http://repository.law.umich.edu/mlr_fi/vol107/iss1/10
- Ozawa S, Stack ML. Public trust and vaccine acceptance-international perspectives. Hum Vaccin Immunother. 2013 Aug;9(8):1774-8. doi: 10.4161/hv.24961.
- Vashishtha VM, Choudhury P, Kalra A, Bose A, Thacker N, Yewale VN, Bansal CP, Mehta PJ; Indian Academy of Pediatrics. Indian Academy of Pediatrics (IAP) recommended immunization schedule for children aged 0 through 18 years—India, 2014 and updates on immunization. Indian Pediatr. 2014 Oct;51(10):785-800.
- Gilson L. Trust and the development of health care as a social institution. Soc Sci Med. 2003 Apr;56(7):1453-68.
- Abelson J, Miller FA, Giacomini M. What does it mean to trust a health system?: A qualitative study of Canadian health care values. Health Policy. 2009 Jun;91(1):63-70. doi: 10.1016/j.healthpol.2008.11.006. Epub 2008 Dec 31.
- De Costa A, Diwan V. “Where is the public health sector?”: Public and private sector healthcare provision in Madhya Pradesh, India. Health Policy. 2007 Dec; 84(2-3):269-76. DOI: 10.1016/j.healthpol.2007.04.004. Epub 2007 May 30.
- Mehrotra S. Caught on camera: for bribes, doctors will prescribe you anything [Internet]. NDTV 2014[cited 2017 Mar 01]. Available from: http://www.ndtv.com/india-news/caught-on-camera-for-bribesdoctors-will-prescribe-you-anything-648170
- Gopichandran V. Trust in healthcare: an evolving concept. Indian J Med Ethics. 2013 Apr–Jun;10(2):79-82.
- Kane S, Calnan M. Erosion of trust in the medical profession in India: time for doctors to act. Int J Health Policy Manag. 2016 Nov 2;6(1):5-8. doi: 10.15171/ijhpm.2016.143.
- Rowe R, Calnan M. Trust relations in health care—the new agenda. Eur J Public Health. 2006 Feb;16(1):4-6. DOI: 10.1093/eurpub/ckl004.
- Gopichandran V, Chetlapalli SK. Dimensions and determinants of trust in health care in resource poor settings—aqualitative exploration. PLoS One. 2013 Jul 16;8(7):e69170. doi: 10.1371/journal.pone.0069170.
- Puliyel J. AEFI and the pentavalent vaccine: looking for a composite picture. Indian J Med Ethics. 2013 Jul–Sep; 10(3):142-6.
- Durant J. Participatory technology assessment and the democratic model of the public understanding of science. Sci Public Policy. 1999;26(5):313-19.DOI: https://doi.org/10.3152/147154399781782329.
- Achenbach J. Why do many reasonable people doubt science? National Geographic Magazine [Internet] March 2015 [cited 2017 Mar 01]. Available from: http://ngm.nationalgeographic.com/2015/03/sciencedoubters/achenbach-text
- Jones MM. In a “post truth” world, evidence and experts matter more than ever. RAND Blog [Internet] [cited 2017 Mar 01]. Available from: www.rand.org/blog/2016/12/in-a-post-truth-world-evidence-andexperts-matter-more.html
- Ioannidis JPA. Why most published research findings are false? PLoS Med. 2005 Aug;2(8):e124. Epub 2005 Aug 30.
- Goldcare B. Bad Pharma. London: Faber and Faber; 2012.
- Heininger U. The success of immunization—shovelling its own grave? Vaccine. 2004 May 7;22(15-16):2071-2.
- Ernst E. Rise in popularity of complementary and alternative medicine: reasons and consequences for vaccination. Vaccine. 2001 Oct 15;20 Suppl 1:S90-3; discussion S89.
- Chaturvedi S, Dasgupta R, Adhish V, Ganguly KK, Rai S, Sushant L, Srabasti S, Arora NK. Deconstructing social resistance to pulse polio campaign in two north Indian districts. Indian Pediatr. 2009 Nov;46(11):963-74. Epub 2009 Sep 3.
- UNICEF/WHO. Understanding barriers to polio eradication in Uttar Pradesh: final report [Internet]. New Delhi; 2006 [cited 2017 Mar 01]. Available from: http://www.comminit.com/files/UnderstandingbarrierstoPolioEradicationEPOSFinalReport.DOC
- Milstien J, David Griffin P, Lee J-W. Damage to immunisation programmes from misinformation on contraceptive vaccines. Reprod Health Matters.1995 [cited 2017 Mar 01 ];3(6):24-8.Published online: 18 Jan 2017. Available from: http://dx.doi.org/10.1016/0968-8080(95)90155-8
- Muhammed S, Nayar KR, Lal SS. Diphtheria deaths in Kerala: signs of an impending crisis. Econ Pol Wkly. [Internet] 2015 Oct 24[cited 2017 Feb 28];50(43).
- Mitra T, Counts S, Pennebaker JW. Understanding anti-vaccination attitudes in social media. Proceedings of Tenth International AAAI Conference on Web and Social Media (ICWSM 2016), 2016:269-78.
- Smith MJ, Ellenberg SS, Bell LM, Rubin DM. Media coverage of the measles-mumps-rubella vaccine and autism controversy and its relationship to MMR immunization rates in the United States. Pediatrics. 2008 Apr;121(4):e836-43. doi: 10.1542/peds.2007-1760.
- Rema N. Conflict of interest on recommendation of immunization schedule? The Times of India [Internet]. New Delhi; 2013 January 13 [cited 2017 Mar 01]; Available from: http://timesofindia.indiatimes.com/home/sunday-times/deep-focus/Conflict-of-interest-onrecommendation-of-immunization-schedule/articleshow/18002445.cms
- Srinivasan S. HPV vaccine trials and sleeping watchdogs. Indian J Med Ethics. 2011 Apr–Jun;8(2):73-4.
- Nimegeer A, Farmer J, West C, Currie M. Addressing the problem of rural community engagement in healthcare service design. Health Place. 2011 Jul;17(4):1004-6. doi: 10.1016/j.healthplace.2011.04.013.Epub 2011 May 7.
- Tindana PO, Rozmovits L, Boulanger RF, Bandewar SV, Aborigo RA, Hodgson AV, Kolopack P, Lavery JV. Aligning community engagement with traditional authority structures in global health research: a case study from northern Ghana. Am J Public Health. 2011 Oct;101(10):1857-67. doi: 10.2105/AJPH.2011.300203. Epub 2011 Aug 18.