ARTICLES
Perceptions of stigma among medical and nursing students and tuberculosis and diabetes patients at a teaching hospital in southern India
Manjulika Vaz, Sandra M Travasso, Mario Vaz
DOI: https://doi.org/10.20529/IJME.2016.003
Abstract
Stigma has a significant impact on the diagnosis of a variety of illnesses, patients’ compliance with treatment and their recovery from these diseases. However, the Indian medical and nursing curriculum has given relatively little attention to recognising and addressing the issue of stigma. This study compared the perception of stigma with respect to tuberculosis (TB) and diabetes mellitus (DM) among medical and nursing students to that among patients with these diseases. The Explanatory Model Interview Catalogue (EMIC) questionnaire was used for all patients and student groups. Focus group discussions were held with only the students to understand their concept of stigma and the challenges they face while addressing stigma, and to explore their role in addressing stigma. The data showed that patients with TB prefer not to disclose their illness, while DM is not perceived of as stigmatising by patients. As a group, medical and nursing students attached excessive stigma to patients with both DM and TB, and this may mean that medical professionals subconsciously do harm through their interactions with patients and the attitudes they project to society. The perceptions of stigma were linked to the patient’s socioeconomic background, apart from the medical condition itself. The students recognised that they lacked the skills to understand and address stigma. We recommend that the subject of stigma be integrated into the curriculum of medical and nursing students.
Introduction
Stigmatising attitudes to disease on the part of health professionals, as well as inappropriate attitudes leading to stigma and gaps in addressing it, have medical and ethical implications. A range of illnesses are widely stigmatised, and stigma has been extensively studied in the cases of leprosy, epilepsy, tuberculosis (TB) and human immunodeficiency virus (HIV)/acquired immune deficiency syndrome (AIDS), apart from mental illnesses (1). The impact of stigma on the diagnosis of illnesses, treatment-seeking, compliance with treatment and extent of follow-up, among other things, has also been well documented. Health-related stigma is defined as a social process or related personal experience characterised by exclusion, rejection, blame or devaluation as a result of an enduring feature of identity conferred by a health problem or health-related condition (2). Stigma can be enacted, endorsed or accepted by one side (the stigmatiser), and be internalised or anticipated by the other (the stigmatised) (3). The issue of stigma has received relatively little attention in the medical and nursing curriculum. However, a growing body of evidence, especially in the areas of HIV and mental health, suggests that health professionals may actually contribute to stigma. A study of stigmatising attitudes across disease groups among medical students in the UK showed that the attitudes of the most experienced medical students were worse than those of the others (4). Studies of interventions involving medical students have shown a change in perceptions and a greater awareness of the stigma attached to mental illnesses, in particular (5).
Stigma can also be seen as part of a wider problem in the health practitioner–patient relationship – the problem of “bias”. This is very often unconscious and like a “blind spot”, and could go beyond the illness and include socio-economic-cultural factors as well (6). The ethical consequences of this on the judgment of the health practitioner, his/her attitude towards the person and the family, and the inevitable reinforcement of such biases among a wider community have not been explored in the Indian context.
TB is an infectious disease that causes millions to suffer from ill health each year and is ranked as the second leading cause of death among infectious diseases, after HIV (7). Of the total number of TB cases worldwide, 2–2.5 million are from India alone (8). Data from India show that there is widespread stigma attached to TB among patients of the disease, and a high percentage of them hide their disease from friends and neighbours. This is more the case among the middle and upper-middle classes than the lower-middle and lower classes (9). At the community level, the important health consequences of non-disclosure of the disease for fear of ostracism and discrimination are delayed diagnosis and treatment. This increases the period of infectiousness and promotes the spread of the disease (10, 11). It has also been found that the attitudes and behaviour of health professionals towards those suffering from TB may lead to even greater stigmatisation of TB patients (12).
While most work on illness-related stigma is on communicable or externally visible diseases, it has been recognised that people with non-communicable diseases, such as cancer, diabetes mellitus (DM), cardiovascular disease and chronic respiratory disease, also face stigma. India, where more than 62 million people are currently diagnosed with DM (13) and DM is said to be growing in epidemic proportions, has been called the “diabetes capital of the world”. The International Diabetes Federation, in its “Call to action”, suggests that millions of people with diabetes face stigma and discrimination. It notes that this promotes a culture of secrecy which can create barriers to services, employment and even marriage, and which may stop patients of diabetes from playing an active role in society. Therefore, an appeal has been made for the reduction of diabetes-related stigma so as to enable these patients to claim their rights and responsibilities (14). There is little literature on stigma and diabetes, though there is a wider sociological and psychological understanding of the impact of all chronic illnesses that affect lifestyle, of which diabetes is one.
The objective of this study was to compare perceptions of stigma with respect to a conventionally stigmatising disease (TB) and a relatively non-stigmatising disease (DM) among medical and nursing students with perceptions of stigma among patients of these two illnesses. Apart from discussions of stigma in relation to HIV and during psychiatric postings, there does not appear to be any formal coverage of stigma in the medical and nursing curriculum.
Methodology
Study design
This was a cross-sectional study using mixed methods, covering medical and nursing students across several years of the curriculum in a tertiary care Christian medical and nursing college in southern India, as well as patients with TB and DM from the same medical college hospital.
The participants’ perceptions of stigma were assessed using the Explanatory Model Interview Catalogue (EMIC) questionnaire, along with a brief sociodemographic questionnaire with some questions on clinical history. The EMIC was chosen because of its simplicity of use, its adaptability to different cultural settings, the fact that it has been used previously in India, as well as the fact that it has been used for different health conditions, including TB (1). It has been used both for self-perception of stigma and community perception of stigma (15). The EMIC has 15 items and a scoring of 0–3 (No, Uncertain, Possibly, Yes) for each item. The scores on each single question were added up to get a composite score. This composite score indicates the perceived stigma. The higher the score, the higher the level of perceived stigma. Some of the qualitative explanations given by TB and DM patients regarding their responses on the EMIC scale were also recorded.
Focus group discussions (FGDs) were held to gain an insight into the understanding of stigma among medical and nursing students, challenges to the perception of stigma, and the consequences of stigma in relation to health and illness. The domains of the EMIC were used to design the qualitative guide for in-depth information on the potential doctors’ and nurses’ broader understanding of stigma in a health setting, their experiences and observations of stigma, challenges to the perception of stigma, consequences of stigma and ways to address it.
Study setting and participants
Three batches of undergraduate medical students (first year, mid-course and final year) and two undergraduate nursing student batches (first year and final year) were covered. The students were from various states in India. English was the medium of instruction and all FGDs were conducted in English.
All patients with TB were either sputum-positive or their disease was confirmed by a physician. Patients with co-morbidities such as DM, cancer, psychiatric illnesses and HIV were excluded. Those with extra-pulmonary TB were not included. Patients who had been cured and were being followed up were included. The patients with DM were enrolled from the outpatient department of endocrinology, the nutritional and lifestyle disorders clinic and from among those admitted as inpatients in the same hospital. All were confirmed patients with DM and those with TB, cancer, psychiatric illnesses and HIV were excluded. To evaluate differences in the perception of stigma between medical/nursing students and patients, going by their composite scores of perceived stigma using the EMIC scale, a minimum sample size of 31 in each of the groups was found to be necessary (at an alpha value of 0.05 and 80% power). We oversampled in both groups to allow for any additional analyses, dropouts and incomplete questionnaires.
Data collection and analysis
All EMIC questionnaires were administered between July and November 2013. Between October 2013 and February 2014, the first author conducted eight FGDs among four groups of medical and four groups of nursing students. The FGDs were conducted till data saturation was reached, ie till no new data seemed to be emerging. Each group consisted of an average of eight participants. Written informed consent was taken from all those who were willing to participate in the study.
The EMIC questionnaires and FGDs were assigned IDs to maintain anonymity. Data entry and analysis was done using SPSS version 21. The responses to each item of the EMIC scale were compared for each disease condition, ie TB and DM, across all the medical and nursing students and the respective group of patients using percentages and the Chi square test. The responses “Yes” and “Probably” were clubbed together to denote acceptance of the statement, while “No” and “Uncertain” were clubbed together to denote non-acceptance of the statement. Analysis was performed of grouped statements under the domains of disclosure (statements 1 and 2), self-esteem (statements 3 and 4), community behaviour (statements 5, 6, 7, 8 and 9), family life (statements 10, 11A, 11B, 12), work life (statements 13 and 14) and medical condition (statement 15). The independent t-test and one-way ANOVA were used to compare values across two groups or multiple groups, respectively. The null hypothesis was rejected at p<0.05.
The FGDs were audio-recorded and transcribed by an external consultant. The transcripts were then reviewed by the interviewer, who listened to the audio recording while reading through the transcripts to check for accuracy. Next, the transcripts were analysed thematically by two researchers simultaneously, using NVivo 9.2 qualitative data analysis software.
Ethics statement
The study protocol was granted ethical approval from the institutional review board of the St John’s Medical College, Bangalore, India (IEC Study Ref. No: 70/2013). The purpose and procedure of the study were verbally explained to participants. All participants signed an informed consent form. In the case of illiterate participants, the signature of a witness was obtained. No monetary compensation was provided to the participants.
Results
Sociodemographic characteristics of participants
Table 1 provides the sociodemographic characteristics of the participants. The patients with DM were older, more educated and more likely to be married than the patients with TB. A very small number in both categories of students (medical and nursing) had a personal history of either TB or DM. However, 65 of the 111 medical students (58.5%) and 38 of the 79 nursing students (48.1%) had a family history of DM, while 3.6% of medical students and 12.6% of nursing students had a family history of TB.
| Table 1: Description of subjects across the study groups | ||||
| Students | Patient groups | |||
| Medical | Nursing | TB | DM | |
| Na | 111 | 79 | 51 | 50 |
| Age (years) (mean, SD) | 22±3 | 19±2 | 36±13 | 51±10 |
| Gender distribution (M/F) | 47/64 | 0/79 | 30/21 | 32/18 |
| Year of study (first/mid/final) | 40/39/32 | 39/0/40 | — | — |
| Personal history of TB/DM | 3/3 | 2/1 | ||
| Family history of TB/DM | 4/65 | 10/38 | — | — |
| Duration of illness (years) (mean, SD) | — | — | 0.5±0.5 | 7.5±6.4 |
| Educational status (£ middle school) | 23 (45) | 15 (30) | ||
| Marital status * (married) | 32 (64) | 47 (96) | ||
| a Total intake of medical students is 60 per year and of nursing students is 100 per year.
* Widowed N = 1 in each group, Numbers indicate the mean and ± indicates standard deviation |
||||
Perceptions of stigma related to TB and DM across study groups
The overall perception of stigma among those with TB was eight times higher than that among those with DM (composite score 9.0±7.1 for TB and 1.2±2.4 for DM). The perception of stigma related to TB was two-and-a-half times higher among the medical and nursing students than among the patients themselves with TB. Similarly, the perception of stigma was seven times higher than that of the patients themselves with DM. There was no significant difference between the perceptions of medical and nursing students both in the case of TB and DM (Table 2).
| Table 2: Distribution of responses for each item of the EMIC scale for TB and DM across the study groups | ||||||
| Statements | Medical students | Nursing students | Patients | |||
| TB | DM | TB | DM | TB | DM | |
| 1. If possible, would you prefer to keep people from learning about your TB/ DM? | 80/110
(72.7) |
50/109
(45.9) |
47/79
(59.5) |
34/76
(44.7) |
36/51
(70.6) |
4/50
(8.0)a |
| 2. Have you discussed this problem with the person you consider the closest to you, the one whom you usually feel you can talk to the most easily? | 7/111
(6.3) |
5/110
(4.5) |
8/77
(10.4) |
1/76
(1.3) |
2/51
(3.9) |
1/50
(2.0) |
| 3. Do you think less of yourself because of this problem? Has it reduced your pride or self-respect? | 61/111
(55.0) |
34/110
(30.9) |
44/78
(56.4) |
15/77
(19.5) |
12/51
(23.5)a |
4/50
(8.0)a |
| 4. Have you ever been made to feel ashamed or embarrassed because of this problem? | 65/111
(58.6) |
25/110
(22.7) |
52/76
(68.4) |
16/76
(21.1) |
7/51
(13.7)a |
0/50
(0)a |
| 5. Do your neighbours, colleagues or others in your community have less respect for you because of this problem? | 45/111
(40.5) |
8/110
(7.3) |
45/78
(57.7) |
9/76
(11.8) |
10/51
(19.6)a |
1/50
(2.0) |
| 6. Do you think that contact with you might have any bad effects on others around you even after you have been treated? | 33/110
(30.0) |
5/110
(4.5) |
19/78
(24.4) |
7/77
(9.1) |
5/51
(9.8)a |
0/50
(0) |
| 7. Do you feel others have avoided you because of this problem? | 77/111
(69.4) |
6/111
(5.4) |
55/79
(69.6) |
7/79
(8.9) |
3/51
(5.9)a |
0/50
(0) |
| 8. Would some people refuse to visit your home because of this condition even after you have been treated? | 60/111
(54.1) |
5/109
(4.6) |
40/78
(51.3) |
5/77
(6.5) |
4/51
(7.8)a |
1/50
(2.0) |
| 9. If they knew about it, would your neighbours, colleagues or others in your community think less of your family because of this problem? | 35/111
(31.5) |
11/110
(10.0) |
30/79
(38.0) |
8/77
(10.4) |
5/51
(9.8)a |
0/49
(0) |
| 10. Do you feel that your problem might cause social problems for your children in the community? | 63/111
(56.8) |
17/109
(15.6) |
46/78
(59.0) |
14/76
(18.4) |
10/50
(20.0)a |
0/50
(0)a |
| 11A. Do you feel that this disease has caused problems for you in getting married? (Unmarried only) | 67/108
(62.0) |
45/108
(41.7) |
44/78
(56.4) |
41/77
(53.2) |
3/16
(18.8)a |
0/2
(0) |
| 11B. Do you feel that this disease has caused problems in your marriage? (Married only) | 52/106
(49.1) |
30/104
(28.8) |
24/62
(38.7) |
17/60
(28.3) |
2/34
(5.9)a |
1/48
(2.1)a |
| 12. Do you feel that this disease makes it difficult for someone else in your family to marry? | 31/111
(27.9) |
20/110
(18.2) |
27/76
(35.5) |
17/76
(22.4) |
3/51
(5.9)a |
1/49
(2.0)a |
| 13. Have you been asked to stay away from work or social groups? | 65/110
(59.1) |
8/110
(7.3) |
47/76
(61.8) |
2/77
(2.6) |
4/51
(7.8)a |
1/50
(2.0) |
| 14. Have you decided on your own to stay away from work or social groups? | 65/110
(59.1) |
13/110
(11.8) |
51/78
(65.4) |
10/77
(13.0) |
25/51
(49.0) |
2/50
(4.0) |
| 15. Because you have TB/DM, do people think you also have other health problems? | 75/111
(69.4) |
82/110
(74.5) |
51/77
(66.2) |
53/77
(68.8) |
4/51
(7.8)a |
0/50
(0)a |
| COMPOSITE SCORES | N=103
21.3a ±6.6 |
N=110
8.3a,b ±5.6 |
N=54
20.4a ±8.1 |
N=57
8.1a,b ±6.7 |
N= 48
9.0 ±7.1 |
N=47
1.2b ±2.4 |
| The numbers indicate Yes + Possibly responses out of the number who responded to that statement, with the percentages indicated in parentheses. The composite scores indicate mean, ± =SD, a = significant difference from corresponding patient group (TB, DM), and b = significant difference between diseases within the subgroups (medical students, nursing students, patient groups). | ||||||
The medical and nursing students’ perceptions of stigma with respect to TB were of a significantly higher level in the case of most of the individual statements of the EMIC questionnaire, as compared to the perceptions of the patients with TB. The exceptions were for statement 1, which relates to a patient’s preference to disclose that he/she has TB, and statement 14, which refers to staying away from work and social groups. In the case of these two statements, the responses were relatively similar.
In the case of DM, there was a significantly high level of stigma attached to the disease by the medical and nursing students. The areas concerned were disclosure of the illness (statement 1), lowered self-respect among people with DM (statement 3), the children of persons with DM facing social problems in the community (statement 10), the disease acting as a barrier to marriage for the person with DM or a family member and a troubled marital life (statements 12, 11A and B), and a perception of greater medical problems (statement 15).
The patients of TB had a lower perception of stigma than did the students because, as they said, “TB is treatable,” and, “People will forget they had it after some time.” DM was seen as a common disease and was associated with affluence. According to one person, “Everyone believes that now diabetes is okay. It’s a trend, like a symbol, moving up the ladder.” Another said, “Every other person has it.” There was some lack of understanding about the sequelae of diabetes, such as diabetic foot and chronic kidney disease, with the patients not fully aware that these are related to diabetes. The student community seemed to have a highly medicalised view of both illnesses.
… he got TB because of lower immunity, so while he is suffering from this disease there are chances of getting other diseases also. (Nursing, Year 1)
People with diabetes are essentially normal on the outside. They may have complications later on, which they wouldn’t really think about that much but per se, they are able to function pretty normally, except for an odd injection or tablet. (Medical, Year 4)
The analysis of subgroups of students showed that first-year medical and nursing students associated TB and DM with greater stigma than did their peers in later years. There was a significant difference between the responses of students in different years with regard to the impact of TB on the patients’ marriage. The number of first-year medical students who believed that patients with TB would have marital problems was twice that of the final-year students who held such a view. First-year nursing students had a three times greater perception than did their senior counterparts that patients with DM would have marital problems.
In the FGDs, junior nursing students explained that family and traditional beliefs influenced the way they thought. First-year students in both the medical and nursing courses were less clear about the aetiology of the diseases than their seniors. The possibility that the students’ perceptions of the stigma faced by these patients were influenced by what they thought were socially appropriate responses cannot be ruled out.
There were no significant differences in the perception of stigma across most items in the EMIC scale between male and female medical students. The exceptions were that there was a sense of shame in the case of TB (statement 4, p<0.05), a perception that the patient’s children would face trouble from the community (statement 10, p<0.05), and the perception that if there was a patient with TB in the household, his/her family members would face problems getting married (statement 12, p<0.05). In the context of these issues, it was the female medical students who overestimated the stigma. In the case of DM, male medical students had a significantly higher perception than female students that those with the disease would receive less respect from the community members (statement 5, p<0.05).
Comparison of perceptions of stigma across six domains across the study groups
Across all domains, there was a significantly lower perception of stigma among the patients with DM than those with TB. The medical and nursing students had a significantly higher perception of stigma than the patients with TB and DM across all domains, except disclosure (domain 1) in the case of TB and the impact of the illness on work life (domain 5) in the case of DM. There was no difference between the perceptions of medical and nursing students across all domains; both groups overestimated the perceptions of stigma to a similar level in the case of the two illnesses.
| Table 3: Composite scores under various domains for the diseases across study groups | ||||||
| Medical students | Nursing students | Patients | ||||
| TB | DM | TB | DM | TB | DM | |
| Domain 1
Disclosure |
N=110
2.2±6.6 |
N=109
1.5a,b±1.3 |
N=77
1.9±1.4 |
N=75
1.3a,b±1.4 |
N=51
2.1±1.4 |
N=50
0.3b±1.0 |
| Domain 2
Self-esteem |
N= 111
3.1a±1.7 |
N=110
1.7a,b±1.9 |
N=75
3.3a±1.8 |
N=76
1.3 a,b±1.7 |
N=51
1.2±1.7 |
N=50
0.3b±0.7 |
| Domain 3
Community behaviour |
N=110
6.1a±3.1 |
N=109
1.1a,b±2.2 |
N=77
6.8a±3.6 |
N=76
1.5a,b±2.6 |
N=51
2.3±3.2 |
N=49
0.1b±0.6 |
| Domain 4
Family life |
N=106
4.2a±2.2 |
N=103
2.0a,b±1.9 |
N=63
3.8a±2.5 |
N=59
2.1a,b±2.2 |
N=48
1.3±2.0 |
N=49
0.2b±0.5 |
| Domain 5
Work life |
N=109
3.4a±1.5 |
N=110
0.6b±1.2 |
N=76
3.3a±1.9 |
N=77
0.5b±1.1 |
N=51
1.7±1.9 |
N=50
0.2b±0.8 |
| Domain 6
Medical condition |
N=111
1.9a±1.0 |
N=110
2.0a±1.0 |
N=77
1.8a±1.0 |
N=77
1.8a±1.2 |
N=51
0.3±0.8 |
N=50
0.1b±0.3 |
| Data indicate mean ±SD; analysis – one-way Anova; a = significant difference from corresponding patient group (TB, DM); b = significant difference between diseases within subgroups (medical students, nursing students, patient groups). | ||||||
What does “stigma” mean to medical and nursing students? (A qualitative exploration)
- Meaning of “stigma” – The words associated with stigma were isolation, rejection, taboo and victimisation. Stigma was associated with circumstances beyond disease. While explaining the word, a fourth-year nursing student said, “They (people) don’t go near widows and they won’t let small children or pregnant women go near a widow – that is stigma. It is isolation” A third-year medical student made the following comparison: “In India, premarital sex would be taboo.”
- Origins of stigma – The themes arising from the discussions on the origins of stigma included those that influenced the participants’ own perceptions as well as those that influenced the community’s perceptions. The primary origin of stigma, according to most students, was ignorance or lack of knowledge and the fear arising out of this. Fear emerged as a critical factor, particularly among the nursing students.
- Perceptions of stigma reflected in health professionals’ action – The healthcare professionals’ perceptions of stigma appear to be influenced by their observations and experiences and fall into two categories. The first of the stigmas is that related to people’s socioeconomic and cultural circumstances, which can be called “social stigma”. This type of stigma takes into account factors such as rural background, literacy levels, housing conditions and so on. The following are a few relevant quotes from the nursing and medical students.
- Challenges to the perception and management of stigma – The students were aware of the need to perceive of the stigma that patients may be experiencing and that addressing the stigma would help in treating them. According to the students, being or feeling stigmatised could be indicated by the body language of the patient, his/her relationships with his/her family members and friends, the patient giving up working, etc. The students acknowledged that the perception and management of stigma were a challenge as they were not equipped to address stigma.
- How to address stigma – The medical and nursing students suggested the following measures to help address stigma.
- Health professionals need to be more empathetic.
- There is a need to avoid re-labelling diseases and one should, instead, address the more deep-seated issues related to disease. Re-labelling a disease, eg leprosy as Hansen disease or HIV as retroviral or “flower case”, does not eliminate stigma.
- There is a need to address issues surrounding the patient, eg family issues, misconceptions of the disease at the community level. This was especially identified by nursing students.
- A good knowledge of the disease is a must to remove fear and prejudice and to learn about and follow universal precautions.
There was only one group – the first-year nursing students – which was not familiar with the word “stigma” in the psychosocial context, and described its botanical meaning (“part of a flower”). Some were also of the view that stigma could be a “false belief” or an “unnecessary fear”. When the group was not familiar with the word “stigma”, the FGD was conducted using the word “rejection” or “discrimination” which emerged from their discussion.
There was this patient with a congenital bone deformity and he wanted to use the toilet in our hospital, but the lady who works in the hospital didn’t let him because she thought it would spread infection. She wanted him to go down to the floor below… (Medicine, Year 3)
Even though they are educated, they still fear the things they are not sure about. They say, ‘Let me be on the safer side.’ Because of a little bit of fear and a little bit of selfishness also, he will not go near that patient or he will try to keep him away and that is where stigma originates… (Nursing, Year 4)
Stereotypes of stigma appear to originate from deep-seated cultural beliefs and traditions, from societal norms, passed on and perpetuated through family dictates, and from media projections. The medical or nursing students were not immune to these influences.
People will stay away from HIV patients and treat them as outcasts. This has developed over the years. .. There are so many other ways in which you can get HIV, but anyone who is HIV-positive is automatically labelled immoral. (Medicine, Year 1)
It’s because our ancestors said it’s not proper, it’s become a stigma. It started and it kept on going the same way. Later, when we started understanding stuff clearly, we realised we don’t need stigma but the behaviour continues. (Nursing, Year 4)
…The media has a big role to play in this. Even in the movies they portray things that are not real or true; they don’t realise that this causes stigma as well. (Nursing, Year 3)
• We consider the people who come from villages as illiterate or unaware of things, so we tend to stigmatise that group.
• If a person speaks a different language, “doctors tend to get frustrated and treat the patient differently and are more rude.
• Mainly those in the slums and illiterate people have TB and all, and are avoided by the people.
The second category of stigmatising behaviour shown by the health professionals was “medical stigma”, ie stigma related to disease and associated fears of acquiring the disease or managing the disease. The following include two quotes from the nursing and medical students.
When dealing with HIV patients, we use double gloves. We wear our mask, which we would really not do with any other patient.”
We have a fear of managing, for example, mental illness, so we try to avoid meeting and communicating with the patient.”
Asking for unnecessary tests – HIV tests for all patients.
Table 4 gives more examples of social and medical stigma as perceived by the medical and nursing students.
| Table 4: Examples of social and disease-related stigma as perceived by students | ||
| Social phenomena | Disease-related phenomena | |
| Enacted by society |
• Rejection due to food habits / culture / religion
|
• Fear of living in same house on patient’s discharge from hospital
|
| Enacted by health professionals |
• People who come from villages are considered illiterate or unaware of things, so that group is stigmatised
|
• Reduced treatment for fear of disease transmission
|
• We need to ask questions about family life, social behaviour and work-related issues, which we are not comfortable or trained to do.
• Addressing stigma needs rapport-building time. In a busy, crowded OPD, it is difficult.
• We tend to focus on the doctor’s role and not function as a people’s person.
• Because of stigma, we can miss the diagnosis completely.
• Put yourself in the shoes of the other person.”
• We should think of the patient as our family member.
• Build a rapport with the patient even if it takes time.
The students rightly felt that it was difficult to teach this and were of the view that it would be easier to imbibe it through good role models.
• They (the community) will not listen to anyone at their own educational level, but if someone of a higher educational level comes and talks to them, they will definitely listen…we are someone great for them.” “We will try to make them (the family) understand … we will tell the father/mother/brother/sister … ‘You take prophylaxis… It will not spread.’ (Nursing, Year 4)
Discussion
The study shows that TB is still stigmatised, as at the level of the patients, their preference is not to disclose their illness. However, the fact that TB is treatable and curable emerges as a major reason for which treatment is sought and the level of stigma has decreased. DM, contrary to a few studies in the West, is not perceived as stigmatising by persons with DM, as assessed using the EMIC scale in this study.
As a group, medical and nursing students had an excessive perception of stigma both with respect to patients with TB and DM. The qualitative data suggested that students stigmatise patients on the basis of social factors, such as a lack of formal education, low economic status and rural background. A few other reasons for their high perceptions of stigma were an unreasonable fear of the transmission of disease, their having witnessed their seniors’ use of gloves and masks, and their having seen their seniors make repeated requests for tests for only certain diseases. These factors could lead to conflict and guilt about focusing excessively on self-protection, and could lead to confusion about which is the right or wrong response. The students acknowledged that patients’ socioeconomic and cultural standing influenced their perceptions. They said that social stigma created a burden for patients insofar as their work and family life were concerned. This coincides with the hidden burden of stigma in relation to illness (16). Within each student group, first-year students associated the conditions with a greater degree of stigma than did their senior peers. This could be due to their limited knowledge of the conditions and their treatment, or their inability to change the situation. Alternatively, their responses could have been driven by the urge to be socially correct. Medical students felt a stronger inability to address the social burden associated with disease than the nursing students. This is possibly because the nursing course covers more of the social sciences and also includes more outreach activities. The FGDs seemed to reveal the existence of unconscious biases among the students and also, a heightened feeling that they would be unable to respond to sources of stigma, whether in the community, within themselves or among their peers. The relatively high perception of stigma among the students could influence their behaviours towards their patients, and this has several ethical implications. Another factor to be noted is that responses to the patient are not always overt and may exist at the level of thoughts and perceptions, which influences the behaviour of healthcare personnel. In the USA, while racial issues appear to be central to the prejudices harboured by doctors, ethnographic studies have shown that responses to social inequality and physical appearance do exist at the unconscious level and are masked due to training or conditioning (17).
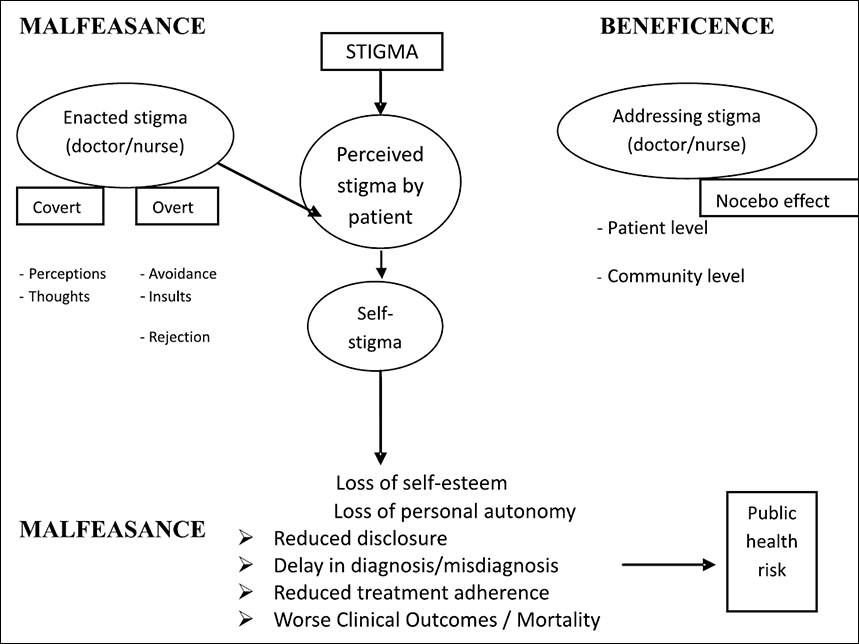
An ethical construct of stigma is presented in Figure 1. The emphasis on responding to the ethical consequences of stigma is derived from the work of the French–Jewish philosopher, Emmanuel Levinas (18). The need for this response is centred around the virtue of “radical responsibility for the other”. This model would be useful to construct teaching methodologies to address the lacunae in the understanding of stigma among medical and nursing students, as seen in this study. It brings to the fore the principles of medical practice, viz to do good (beneficence), to do no harm (malfeasance), and to address the individual (clinical role) as well as community role (societal role). This model questions the ethics of a passive acceptance of something that appears beyond one’s control but has significant potential for harm. This is important in the context of the current study since the students recognised the connect between stigma and disease, but felt powerless to do anything about it. The model calls for an understanding of stigma beyond biomedicine and within a sociocultural system. The construct also takes elements from the sociological model of Erving Goffman (19), in which stigmatisation is a social process resulting from interpersonal interactions. However, a key point to note is the health professional’s role in either alleviating or exacerbating the felt stigma through his/her interactions with the patient or patient’s family.
When an illness is socially stigmatised and stigma is enacted against patients by people in high positions (eg doctors), the stigma has a greater chance of becoming internalised. As a consequence of this, a process of self deprecation and “self stigma” occurs even without an external stigmatizing behavioural trigger. (20, 21).
By overestimating the stigma attached to the two diseases, there is a possibility that health professionals actually do harm (malfeasance), both in their interactions with patients and the attitudes they project to society. Health practitioners are extremely influential and held in high regard in society, so their attitude has a snowball effect on the community, which wishes to emulate them.
In this schema, the stigma enacted by the health professional against the patient could be covert (in the form of thoughts, perceptions and indirect behaviour), or overt (in the form of avoidance, insults and rejection). When stigma becomes internalised, the consequences of self-stigma are often a loss of self-esteem and a loss of autonomy (22). These may result in a decrease in the disclosure of illness, a delay in diagnosis or the initiation of treatment, reduced adherence to treatment, a fall in the quality of life and a worsening of the prognosis of the disease. Apart from the impact on the individual patient, there is a risk to the person’s family and the larger community in the case of a communicable disease. If health professionals inadvertently ally themselves with the family or community in a manner that is discriminatory towards the patient, they will only perpetuate the stigmatising effect (20).
Addressing issues of stigma goes beyond the formal line of biomedical “duty”. One must spend time to explain the illness to the patient and educate him/her on it, be alert to a possible “Nocebo” effect (23), ie the effect that negative news can have on one’s health, and address observed prejudices and stigmatising behaviour among the patient’s peers, colleagues and caregivers. Disclosure of the illness to the patient’s family members is another dilemma for the health professional in the case of a stigmatising illness. Does one respect the wishes of the patient and put the others at risk? Should one suppress the wishes of the individual for the sake of the greater public good? There is also the effect of “courtesy stigma”, described by Goffman as the rub-off effect of stigma from the discredited individual to the family (20). Counselling the patient and caregivers and being there in case of a negative fallout require time, effort and going beyond a comfort zone that is traditionally defined by the health professional.
Stigma is not just a process of labelling that hinders treatment and creates a public health risk, but is in a sense, an infringement of human rights, which requires a response. To help eliminate stigma, the health professional, whether a doctor or nurse, has to be an agent of social change, address issues of discrimination, stand up for social justice and acknowledge that the voices of a minority (in this case, the stigmatised), however small, are not insignificant.
In Levinas’ paradigm on stigma, “radical responsibility for the other” suggests that we must go beyond recognising and understanding the issues related to stigma; we must commit ourselves to doing something about it and realise that stigma, even if experienced by the other, is our responsibility. Hence, we recommend incorporating the topic “Handling stigma in illness – the role of the health professional” in the medical and nursing curriculum for undergraduate students. While various other studies and reviews of health-related stigma have recommended interventions at the community level, in public health research and in social and health policy, our view is that interventions in the curriculum, which is taught during the formative years, will equip health professionals to have the sensitivity and skills required to reduce stigma and avoid exacerbating it both at the subconscious and conscious levels.
Conclusions
The main finding of this study is the excessive stigma attached by medical and nursing students to patients with TB and DM. The stigma appears to be related to socioeconomic conditions, such as the class, educational level and living conditions of the patient more than the illness per se. Precautionary measures, such as wearing of gloves and masks, are often confused with discriminatory behaviour and stigma. While a greater knowledge of the disease would help to improve the clinical judgment of health professionals, the higher perception of stigma among them could influence their behaviour towards their patients, and this has several ethical implications. We feel that there is a need to provide students with a socio-cultural-ethical understanding of stigma, and to increase their sensitivity and skills so that they can address discriminatory biases within themselves and their peers, towards their patients, and towards the public. We recommend that the topic “Handling stigma in illness – the role of the health professional” be included in the undergraduate curriculum of medical as well as nursing students. An ethical response on the part of the doctor or nurse to discrimination against “the other” will go a long way in addressing stigma and its adverse consequences.
Acknowledgements
We acknowledge the role of Ms Priya Shetty of St John’s Research Institute and Ms Usha Shetty, who helped with the collection of data from the TB and DM patients. Ms Priya Shetty also translated the informed consent form from English into Kannada. In addition, we would like to thank the Department of Chest Medicine, the local DOTS centre, the Department of Endocrinology and The Nutrition and Life Style Clinic at St John’s Medical College Hospital, Bangalore for helping us reach the patients.
Competing interests statement: All the authors declare no competing interests.
Funding statement: The study was funded through a research grant from The Research Society, St John’s Medical College, Bangalore (grant ref. no. RS/1/10713).
Previous similar submissions: All authors declare that no previous submissions of similar work have been made to any other journal.
References
- Van Brakel WH. Measuring health related stigma – a literature review. Psychol Health Med. 2006;11(3):307-34.
- Weiss MG, Ramakrishna J. Stigma interventions and research for international health. Lancet. 2006;367:536-8.
- Scrambler G. Stigma and disease: changing paradigms. Lancet. 1998;352(9133):1054-5.
- Korszun A, Dinos S, Ahmed K, Bhui K. Medical student attitudes about mental illness: does medical-school education reduce stigma? Acad Psychiatry. 2012;36(3):197-204.
- Schmetzer AD, Lafuze JE, Jack ME. Overcoming stigma: involving families in medical student and psychiatric residency education. Acad Psychiatry. 2008;32(2):127-31. doi: 10.1176/appi.ap.32.2.127.
- Adams V, Kaufman SR. Ethnography and the making of modern health professionals. Cult Med Psychiatry. 2011;35(2):313-20. doi: 10.1007/s11013-011-9216-0.
- Kassam A, Glozier N, Leese M, Loughran J, Thornicroft G. A controlled trial of mental illness related stigma training for medical students. BMC Med Educ. 2011;11:51. doi: 10.1186/1472-6920-11-51.
- World Health Organization. Global Tuberculosis Report 2013. Available from: http://www.who.int/tb/publications/global_report/en/
- World Health Organization. Tuberculosis control in South-East Asia Region. Regional Report, 2013.
- Dhingra VK, Khan S. A sociological study on stigma among TB patients in Delhi. Indian J Tuberc. 2010;57(1):12-18.
- Courtwright A, Turner AN. Tuberculosis and stigmatization: pathways and interventions. Public Health Rep. 2010;125 Suppl 4:34-42.
- Jackson L, Yuan L. Family physicians managing tuberculosis. Qualitative study of overcoming barriers. Can Fam Physician. 1997;43:649-55.
- Dodor E. Health professionals expose TB patients to stigmatization in society: insights from communities in an Urban district in Ghana. Ghana Med J. 2008;42(4):144-8.
- Kaveeshwar SA, Cornwall J. The current state of diabetes mellitus in India. Australas Med J 2014;7(1):45-8. doi: 10.4066/AMJ.2013.1979. eCollection 2014.
- International Diabetes Federation. A call to action on diabetes, November 2010.
- Weiss MG, Ramakrishna J, Somma D. Health-related stigma: rethinking concepts and interventions. Psychol Health Med 2006;11(3):277-87.
- Hannah SD, Carpenter-Song E. Patrolling your blind spots: introspection and public catharsis in a medical school faculty development course to reduce unconscious bias in medicine. Cult Med Psychiatry. 2013;37(2):314-39. doi: 10.1007/s11013-013-9320-4.
- Sebastian SS. Radical Responsibility for the other: an ethical appraisal of Emmanuel Levinas. Bangalore: Asian Trading Corporation; 2010.
- Goffman E. Stigma: notes on the management of spoiled identity. New York: Simon and Schuster; 2009.
- Corrigan PW, Watson AC. Understanding the impact of stigma on people with mental illness. World Psychiatry. 2002;1(1):16-20.
- Vogel DL, Wade NG, Hackler AH. Perceived public stigma and the willingness to seek counseling: the mediating roles of self-stigma and attitudes toward counseling. J Couns Psychol. 2007;54(1):40-50. Available from: http://dx.doi.org/10.1037/0022-0167.54.1.40
- Weiss M. Explanatory Model Interview Catalogue (EMIC): framework for comparative study of illness. Transcultural Psychiatry. 1997;34(2):235-63.
- Benson H. The Nocebo effect: history and physiology. Preventive Medicine. 1997;26(5):612-15.