COMMENTS
Ethics of dental health screening
Chandrashekar Janakiram, Farheen Taha
DOI: https://doi.org/10.20529/IJME.2016.047
Abstract
Screening is the detection of disease at a point in its natural history when it is not yet symptomatic. In the natural history of dental caries, for example, the incipient lesions are at a reversible stage, which is a pre-symptomatic or an unrecognised symptomatic disease. Ideally, this is the stage during which screening should identify the risk of dental caries; however, presently, the so-called dental screening employed identifies the clinical cavitation of the tooth, which is very obvious to the individual. The individual already knows that he/she has dental caries and needs treatment, which the screening personnel (dental doctor) explains again during the screening procedure. Is it ethical to call such an event screening? The mushrooming of dental teaching hospitals has promoted regular screening of dental diseases among the communities and schoolchildren through their community dentistry-related activities. More often, it is a dental “check-up” that is carried out on the pretext of screening for dental diseases. Though the basic intention of this activity is to promote awareness of dental diseases and promote good health, there is also a hidden agenda to it. An artificial demand for dental care is created that is easily capitalised on by the dental teaching institutions to enhance its clinical activity. Dental screening is doing more harm than good as patients are made aware of the diseases for which they may not be able to afford treatment. This narrative review gives an account of the scientific evidence on screening for oral diseases, the current practices in screening and the ethical dilemmas of dental screening programmes.
Introduction
Screening is the embodiment of preventive programmes. It is the search for unrecognised sickness or defect by means of rapidly applied tests, examinations and other procedures in apparently healthy individuals (1). The Conference on Preventive Aspects of Chronic Disease, held in 1951, defined screening as “the presumptive identification of unrecognised disease or defect by the application of tests, examinations, or other procedures which can be applied rapidly. Screening tests sort out apparently well persons who probably have a disease from those who probably do not. A screening test is not intended to be diagnostic. Persons with positive or suspicious findings must be referred to their physicians for diagnosis and necessary treatment” (2). “Screening is a method used for the detection of a disease at a point in its natural history when it is not yet symptomatic. The ability to screen for a particular disease is contingent on the disease having a detectable preclinical phase that is long enough to permit its early detection. The logic of screening is that the early detection of disease may alter the natural course of the disease and prevent the onset of adverse outcomes” (3).
History of dental screening
Dental screening began in the year 1918 in the United Kingdom, when school dental inspection, with subsequent treatment if necessary, was written into the Education Act. Later in 1964, the Department of Health, United Kingdom, defined this activity as “identifying children in need of treatment”. However, in 1986, this activity came to be known as “dental screening” (4).
Despite great achievements in the overall health of the populations around the globe, according to recent reports from the World Health Organization, oral diseases are still widely prevalent worldwide. This is so particularly among underprivileged groups in the developed and developing countries (5). Oral diseases such as dental caries, periodontal diseases, tooth loss, oral mucosal lesions and oropharyngeal cancers, human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS)-related oral diseases and oro-dental traumas are a cause of major public health problems worldwide (6). Dental caries and periodontal diseases have historically been considered the most important global oral health burdens. Dental caries still affects 60%–90% of schoolchildren and the vast majority of adults (5), sometimes even as high as 100% of adults (6). In most developed nations, access to dental care is very limited and the carious teeth are left untreated or are extracted due to pain. Edentulousness among adolescents and young adults is a common occurrence. Most children have some form of gingivitis, and severe periodontitis and resultant tooth loss is seen in 5%–15% of the adult population (5). The situation is graver still as, according to Leake et al, in the future, access to dental care may worsen in most countries as trends in demography, disease and development come to bear on national oral healthcare systems (7). All these factors, along with the recent fad of “prevention being better than cure” and, of course, the very favourite proverb “a stitch in time saves nine”, have led to a torrent of oral disease screening programmes worldwide.
Principles of screening
In the mid-1960s, Wilson and Jungner (2) had put forward certain principles of screening. They were important guidelines for planning screening programmes (2, 8):
- The condition sought should be an important problem.
- There should be an acceptable means of treating patients with recognised disease.
- Facilities for diagnosis and treatment should be available.
- There should be a recognised latent or early symptomatic stage.
- The natural history of the condition, including its development from latent to declared disease, should be adequately understood.
- There should be a suitable test or examination.
- The test or examination should be acceptable to the population.
- There should be an agreed policy on those who are to be treated as patients.
- The cost of case-finding (including diagnosis and the subsequent treatment of patients) should be economically balanced in relation to the possible expenditure as a whole.
- Case-finding should be a continuous process and not a “once and for all” project.
Although it is virtually impossible to fulfil all 10 principles to everyone’s satisfaction, most of the principles have to be satisfied. According to Wilson and Jungner, there is no hierarchy of importance among the principles, but the ability to treat the condition adequately when discovered is probably paramount (8).
Does the present dental screening programme satisfy this paradigm?
Tickle and Milsom say in their article that oral screening does not satisfy the criteria set forth by Wilson and Jungner. In fact, it does not even fit the definition or description of screening (4), since oral screening involves just a visual inspection of each child’s mouth. It is performed under suboptimal conditions, under poor lighting and with the subjects poorly positioned. The sophisticated diagnostic tests, such as radiography and transillumination, are not employed. In such scenarios, the detection of early disease is virtually impossible. Also the “screening test” is not standardised. The activity has no specific aims and objectives, and the dentists performing screening are not usually calibrated (4). Even if people are screened one way or another, most of the time there is no adequate follow-up, or the people do not avail themselves of dental treatment if they are screened positive. Thus, the screening procedures are deemed unproductive. A cluster randomised control trial by Tickle et al demonstrated how the school dental screening programmes have no effect whatsoever on reducing untreated dental caries in either primary or permanent dentition and on increasing dental attendance rates among children living in urban communities in the northwest of England (9).
According to Tickle’s study, only 32.1% of the children who were screened consulted a dentist during the follow-up period, compared to 37.6% of the group that was not administered any screening procedure. Furthermore, Tickle stated that dental screening was not effective in stimulating dental attendance at the population level. Tickle et al also conducted another prospective cohort study during the same time and the results of that study showed that screening has a minimal impact on dental attendance and only a small proportion of screened positive children receive appropriate treatment.
In another cluster randomised controlled trial by J Rodgers, there were four arms. One arm had the traditional screening method, another arm a new model of screening, a leaflet arm and a control arm. Although the attendance rates in the two screened arms were 42% and 41% compared to 38% in the control arm, these differences were not statistically significant (10). This only further reinforced that school dental screening delivered according to three different models was not effective in reducing the levels of active carious lesions and in increasing dental attendance among the populations under study. In their study, Cunningham et al also demonstrated the ineffectuality of the screening programmes in which, apart from normal screening, even a personalised letter to the guardian did not yield any significant results as far as the dental attendance rates were concerned. In fact, neither the two dental inspection methods, nor sending a letter to the children’s homes resulted in a rise in the follow-up rates in 12–13-year-olds, compared to a control group of children who received no intervention at all (11).
A cross-sectional questionnaire study by Tickle et al showed that most school dental screening programmes do not collect sufficient data to evaluate the impact of their programmes on children’s oral health (12). Moreover, a review by Morgan et al confirmed that the Community Dental Service managers in England and Wales view dental screening as a vehicle to increase dental registration among schoolchildren (13). Morgan also says that a qualitative study by Preston et al (14) documented that many parents see dental health and the need to attend a dentist, once prompted by screening, as a low priority in the day-to-day lives of families with young children. The parents feel that it is the responsibility of the people administering the screening to ensure treatment afterwards.
This does not usually take place, since those administering the screening wash their hands of the children once a letter is sent home. The parents also feel that these screening programmes are akin to “policing” them and forcing them to do something they are not comfortable with (14).
There are considerable financial dilemmas associated with screening. In 1992 alone, the NHS in the UK spent £ 2.5 million on the screening of schoolchildren (4). One can only imagine the present-day burden these programmes are placing on the economy of the country, especially since the recent years of recession and consequent financial crisis (15). Throughout the 20th century, the exact role of school dental screening was never defined. In order to maintain its continued existence, the policy-makers adopted a pragmatic approach and kept changing the model to fit the ever-changing dental landscape. School dental screening has enjoyed a lot of political support in the UK and in many countries around the globe. It is seen as a key dental public health intervention. The literature, especially in the western countries, says that while the concept of dental screening is attractive to policy-makers, there is no scientific evidence that it helps improve the oral health status of children or the adult population (16).
Ethics of screening
Although screening is said to yield benefits in the case of many medical conditions, such as diabetes mellitus and phenylketonuria, there seems to be a wide gap in screening for oral diseases such as dental caries and periodontal diseases. Mixed opinions have been expressed on the effects of dental screening on the outcome or progression of oral diseases. A study by Edelstein et al had demonstrated that microbial screening may be useful for the identification of young children infected with cariogenic microorganisms, so that preventive and therapeutic treatments can be tailored to the needs of individual patients (17). At the same time, the literature does quote the futility of mass screening, especially since the treatment aspect is so tactfully ignored in most of the screening programmes (1).
Since the concept of “prevention is better than cure” has become so popular amongst clinicians and the public alike, there has been an avalanche of various types of screening programmes. These programmes are so popular that in the UK, the “school dental screening programme” has become a statutory requirement since the past one hundred years (16). These screening programmes are amongst the most debated aspects of the healthcare system and public health practices, as well as health policy discussions. Although in 1960, the American Public Health Association strongly endorsed multiple screening in its publication titled “Chronic Disease and Rehabilitation: a Program Guide for State and Local Health Agencies”, it recognised that screening should come only second to periodic health examinations as the effective method for early disease detection (2). There are also many ethical, political and philosophical dilemmas related to these screening programmes and this has become the focus of debate in many healthcare settings. Most of the screening programmes thwart all the four principles of ethics put forward by Beauchamp and Childress, i.e. beneficence, non-maleficence, justice and autonomy (18). Beneficence is more for the organisations or institutions that conduct these screening programmes. Although those who are screened positive are benefitted as far as knowing their dental status is concerned, this advantage is not very significant since they were already aware of their dental health status. Non-maleficence and justice are also affected since the individual is made aware of his/her disease condition, for which he/she may or may not be provided treatment. Most of the time, it is a one-way ticket to disheartenment.
The screening programmes have the potential to violate each of these principles. Many a time, patients are coerced into screening by doctors or by publicity campaigns that stress population results more than individual benefits. These population results are achieved only by a high uptake of people which, in turn, is obtained mostly by persistent call and recall systems that send reminders to patients, telling them when their screening is due. Patients may interpret the content of these letters as the decision having been made for them and, therefore, the abdication of their right to informed consent. Many participants believe that the screening procedures, the risks/benefits of which they are not informed, are unethical.
Cochrane and Holland (19) describe this fallacy in a very apt manner: “We believe that there is an ethical difference between everyday medical practice and screening. If a patient asks a medical practitioner for help, the doctor does the best he can. He is not responsible for defects in medical knowledge. If, however, the practitioner initiates screening procedures, he is in a very different situation. He should, in our view, have conclusive evidence that screening can alter the natural history of the disease in a significant proportion of those screened. “Most of the time, deprived and vulnerable people who are at greater risk of certain diseases are less likely to undergo screening interventions. Screening programmes can actually increase the health gap if a higher fraction of those with better health determinants are covered while vulnerable people remain untouched by the programme (20). Also, screening raises the question, “Is the person healthy after all?” This creates unnecessary panic and anxiety, however short-lived, until the result shows negative.
Moreover, it is not always easy to make a distinction between those individuals who have a disease and those who do not, even with the help of a gold standard. Introducing and implementing a screening programme is expensive and involves a large number of people. The cost of the screening programme (including testing, diagnosis and treatment, administration, training and quality assurance) should be economically balanced in relation to the expenditure on medical care as a whole. Economic evaluations should be subject to sensitivity analysis and discounting. This is not the case most of the time (18).
Clinicians are also frustrated when patients are reluctant to comply with the screening procedures because they are apprehensive about the procedures, do not like to be put in the position of a “patient” or simply do not trust the evidence. In these cases, clinicians might come across as overbearing and try to convince the patients of the pros and cons of the procedure. However, one must comprehend the fact that the autonomy of the patient is at stake here and it must be recognised that it is not unreasonable to value some choices over others (21). It is of critical importance to consider ethical issues in planning a screening programme so as to ensure that the main focus of screening, which is preventing morbidity, is maximised. There are many crucial lessons to be learnt from the many screening programmes that have been conducted worldwide (22).
Dental screening programme in India
Since oral diseases in India are primarily due to poor oral hygiene, sociocultural factors, inappropriate use of fluorides, lack of knowledge of oral health and poor access to dental care, a three-tier system has been devised to address these problems. The primary intervention is a school-based oral health promotion programme. The secondary strategy is to devise a good oral screening programme and to increase access to dental care (23). Although screening programmes have become very popular in the Indian subcontinent, subsequent treatment or dental care to those who screened positive is infrequent.
The Tamil Nadu government implemented a school screening programme, which received good coverage in a popular newspaper. However, other than the fact that free treatment would be provided to those who screened positive, no other initiative to ensure treatment was mentioned (24).
Among non-governmental organisations, dental screening camps are a popular and sometimes the only means to address oral health. In most situations, no follow-up is provided. In 2010, the Indian Dental Association in Coimbatore organised a screening camp which held the Guinness record for the highest number of people screened in 24 hours. The people screened positive were referred to the dental clinics of the participating dental surgeons. It was said that the extractions and fillings would be provided free of cost, but the full price would be charged for all other procedures (25). Although the study by Hebbal et al showed that the oral screening programme in the Davengere district in India significantly improved the percentage of schoolchildren who sought dental care (26), there is still a dearth of evidence regarding such screening programmes in the country.
Even though there are studies around the rest of the world that consider screening programmes a fallacy (4, 9, 11, 16, 22, 27, 28), we need to carry out further studies in the Indian context to refute or confirm the same. In the natural history of dental caries, for example, the incipient lesions are at a reversible stage, which is a pre-symptomatic or an unrecognised symptomatic disease (Figure 1). Ideally, this is the stage where screening should identify the risk of dental caries. However, at present, the so-called dental screening employed identifies the clinical cavitation of the tooth, which is very obvious to the individual. The individual already knows that he/she has dental caries and needs further treatment. The same information is explained to the individual by the screening personnel (dental doctor) during the screening procedure. Is it ethical to term such an event screening? What is the purpose of such screening? Usually, the outcomes of these screening programmes are that these individuals are referred to the screening personnel’s dental teaching facilities, where they may or may not be provided free treatment.
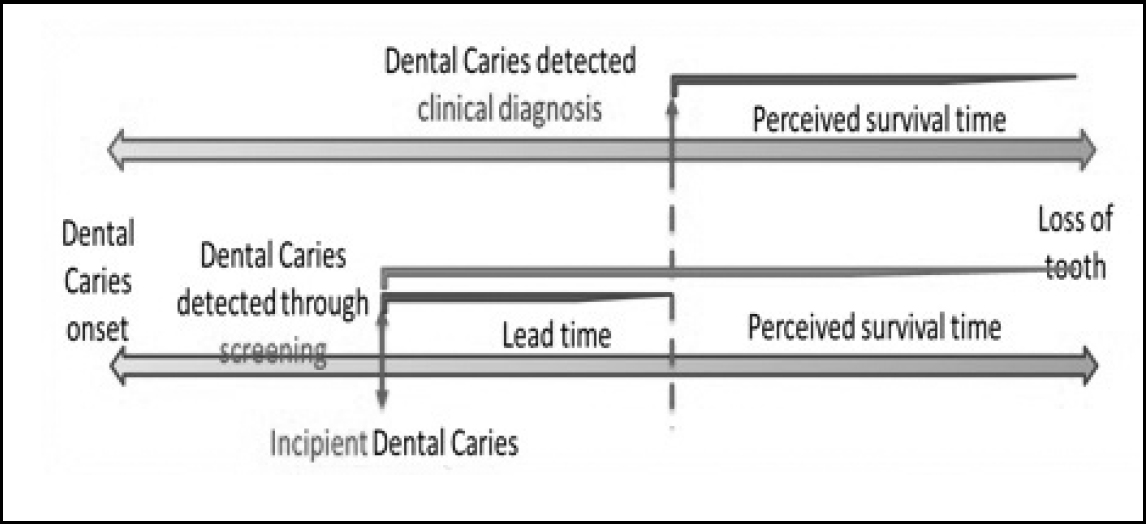
There is sufficient lead time if the screening for dental caries is done when the problem is at the incipient lesion level, rather than when the clinical symptoms are obvious and there are frank carious lesions – this is usually the norm of screening for dental caries in India. There will also be no lead time bias since the dental caries can be altered through treatment as the incipient lesions are usually reversible.
Basically, screening is carried out to convert the normative dental needs of individuals to felt needs, which would increase the demand for dental care which, in turn, is unnecessary. The recent mushrooming of dental teaching institutions has promoted regular screening for dental diseases among the communities and schoolchildren through their community dentistry-related activities. More often, it is dental check-ups that are carried out rather than screening. The basic intention of screening is to promote awareness of dental disease and good health. However, the hidden agenda is to create a demand for dental care and find cases for the clinical activity of dental institutions.
Conclusion
The screening of oral diseases like dental caries and periodontal diseases does not follow the principles of screening. The present school oral health and communitybased screening programmes are carried out to convert the normative dental needs of individuals to felt needs which would ultimately increase the demand for dental care. Dental screening does more harm than good as patients are made aware of diseases which they do not have the time to treat and for which they may not be able to afford the treatment. The demand that is created for dental care is easily capitalised on by dental teaching institutions for enhancing their clinical activity. Screening for oral diseases is sometimes reduced to a farce and it is recommended that it undergo a massive revamp.
Recommendations
- We suggest that if at all a screening programme is to be implemented, it should be done using transilluminators, radiographs and other sophisticated techniques, which can aid in diagnosing incipient lesions and not just frank carious lesions. Our argument in the strictest sense is that “dental health screening” is a “misnomer” which does not fit into the screening criteria. Hence, we should utilise the term “dental check-up” instead.
- We also recommend the establishment of school dental clinics within the school premises that will provide preventive and curative treatment to all children enrolled in the school.
References
- Park K. Park’s textbook of preventive and social medicine. 19th ed. Jabalpur, India: Banarasidas Bhanot Publishers; 2007:p.12-47.
- Wilson JMG, Jungner G. Principles and practice of screening for disease. Public health papers No. 34. Geneva: WHO;1968:26-39.
- Deep P. Screening for common oral diseases. J Can Dent Assoc. 2000;66(6):298-9.
- Tickle M, Milsom KM. Oral screening: time for a change of terminology and methodology. J Med Screen. 1999;6(3):163-4.
- World Health Organization. What is the burden of oral disease? WHO; 2014.
- Petersen PE, Bourgeois D, Ogawa H, Estupinan-Day S, Ndiaye C. The global burden of oral diseases and risks to oral health. Bull World Health Organ. 2005;83(9):661-9. Epub 2005 Sep 30.
- Leake JL, Birch S. Public policy and the market for dental services. Community Dent Oral Epidemiol. 2008;36(4):287-95. doi: 10.1111/j.1600- 0528.2008.00438.x.
- Shickle D, Chadwick R. The ethics of screening: is “screeningitis” an incurable disease? J Med Ethics. 1994 Mar 1;20(1):12-18.
- Milsom K, Blinkhorn A, Worthington H, Threlfall A, Buchanan K, Kearney-Mitchell P, Tickle M. The effectiveness of school dental screening: a cluster-randomized control trial. J Dent Res. 2006 Oct;85(10):924-8.
- Rodgers J. School dental screening does not increase dental attendance rates or reduce disease levels. Evid Based Dent. 2007;8(1):5-6.
- Cunningham CJ, Elton R, Topping GV. A randomised control trial of the effectiveness of personalised letters sent subsequent to school dental inspections in increasing registration in unregistered children. BMC Oral Health. 2009 Mar 12;9:8. doi: 10.1186/1472-6831-9-8.
- Threlfall AG, Milsom K, Catleugh M, Kearney-Mitchell P, Blinkhorn A, Tickle M. A survey of school dental screening practise in community dental services of England and Wales in 2003. Community Dent Health. 2006 Dec;23(4):236-8.
- Morgan M, Bennett H. Dental health screening- an overview of the literature. Chief Dental Officer; September 6, 2013.
- Preston ST, Davies GM, Craven R. An investigation of parents’ attitudes to dental health and school dental screening. Community Dent Health. 2001 Jun;18(2):105-9.
- Kasturi Rangan V, Petkoski DB. Coming out of recession: the role of business in alleviating poverty. Development Outreach. December 2009.
- Milsom KM, Tickle M, Blinkhorn AS. Is school dental screening a political or a scientific intervention? J Dent Res. 2008;87(10):896-9.
- Edelstein B, Tinanoff N. Screening preschool children for dental caries using a microbial test. Pediatr Dent. 1989 Jun;11(2):129-32.
- Beauchamp TL, Childress JF. Principles of biomedical ethics. 5th ed. Oxford University Press; 2001.
- Cochrane AL, Holland WW. Validation of screening procedures. Br Med Bull. 1971 Jan 1;27(1):3-8.
- The Association of Faculties of Medicine of Canada. A virtual textbook on Public Health concepts for clinicians. Part 3 – Practice: Improving Health, Chapter 9 Screening – ethical issues particular to screening. AFMC Primer on Public Health Population.
- Plutynski A. Ethical issues in cancer screening and prevention. J Med Philos. 2012 Jun;37(3):310-23. doi: 10.1093/jmp/jhs017. Epub 2012 May 7.
- Delatycki MB. The ethics of screening for disease. Pathology. 2012 Feb;44(2):63-8. doi: 10.1097/PAT.0b013e32834e8496.
- Lin S, Mauk A. Oral health: addressing dental diseases in rural India. Implement Public Health Interventions in Developing Countries; 2012:105-29.
- School dental health programme launched. The Hindu [Internet], Tambaram, 2001 Jun 22 [cited 2014 Dec 5]. Available from: http://www.thehindu.com/todays-paper/tp-national/tp-tamilnadu/school-dentalhealth-programme-launched/article2124869.ece
- Massive dental screening camp to set Guinness record. The Hindu [Internet], Coimbatore, 2010 Oct 8[cited 2014 Dec 5]. Available from: http://www.thehindu.com/todays-paper/tp-national/tp-tamilnadu/massive-dental-screening-camp-to-set-guinness-record/article819188.ece
- Hebbal M, Nagarajappa R. Does school-based dental screening for children increase follow-up treatment at dental school clinics? J Dent Educ. 2005 Mar 1;69(3):382-6.
- Wallace EA, Schumann JH, Weinberger SE. Ethics of commercial screening tests. Ann Intern Med. 2012 Nov 20;157(10):747-8.
- Milsom K. School dental screening–what value? Br Dent J. 1995;178(9):322.