ARTICLES
An appraisal of the tuberculosis programme in India using an ethics framework
Giridhara R Babu, Sathyanarayana TN, Anant Bhan, J K Lakshmi, Megha Kishore
DOI: https://doi.org/10.20529/IJME.2014.004
Abstract
This is a review of the manner in which the Revised National Tuberculosis Control Programme (RNTCP) is being implemented, with a focus on the attention being paid to ethical principles and the incorporation of these into the programme. The article elucidates how ethical principles can be applied to protect the rights of the potential beneficiaries of the RNTCP. The authors consider the RNTCP in the light of a framework that is usually applied in research to evaluate ethical principles in public health practice. The three key principles of the framework are: respect for persons, beneficence and justice. The authors propose that this framework be used to make an ethical evaluation of other pu health programmes at several levels, since this could bring farreaching benefits to society.
Introduction
Public health professionals constantly face ethical dilemmas in their practice. Moral standards that distinguish right from wrong are based on societal prescriptions, philosophy, values and religious beliefs. Some of these are transmuted into ethical guidelines set by professional bodies. Respect for persons, beneficence (subsuming non-maleficence) and justice form the trinity of principles that comprises one of the most widely prevalent frameworks to guide ethical behaviour: principlism. There is often an implicit expectation that such principles and frameworks be integrated into the design and implementation of public health programmes (1).
It is usually easier to take a clear ethical position in extreme cases, such as that of a patient’s death following gross negligence by medical practitioners or the deliberate and prolonged lack of response to a public health need by the authorities. However, it is more difficult to take a clear position in cases in which injustice or exploitation may not be immediately apparent or explicit, for instance, if a child dies or is disabled as a result of adverse events following immunisation. A clear understanding of ethical principles can aid in the resolution of such dilemmas (2).
Objective
The purpose of this paper is to examine a framework of ethical principles often applied in the context of research – respect for persons, beneficence and justice – and explore its applicability to public health practice. Specifically, we utilise this framework to critically examine the Revised National Tuberculosis Control Programme (RNTCP) in India from the perspective of ethics.
Methods
We studied the published literature, reports of ongoing national programmes and documents outlining ethical principles that have been published by international organisations (3, 4, 5, 6, 7, 8, 9). For the purposes of this paper, public health practice is defined as “any engagement of public health professionals for implementation of public health programmes”(2).
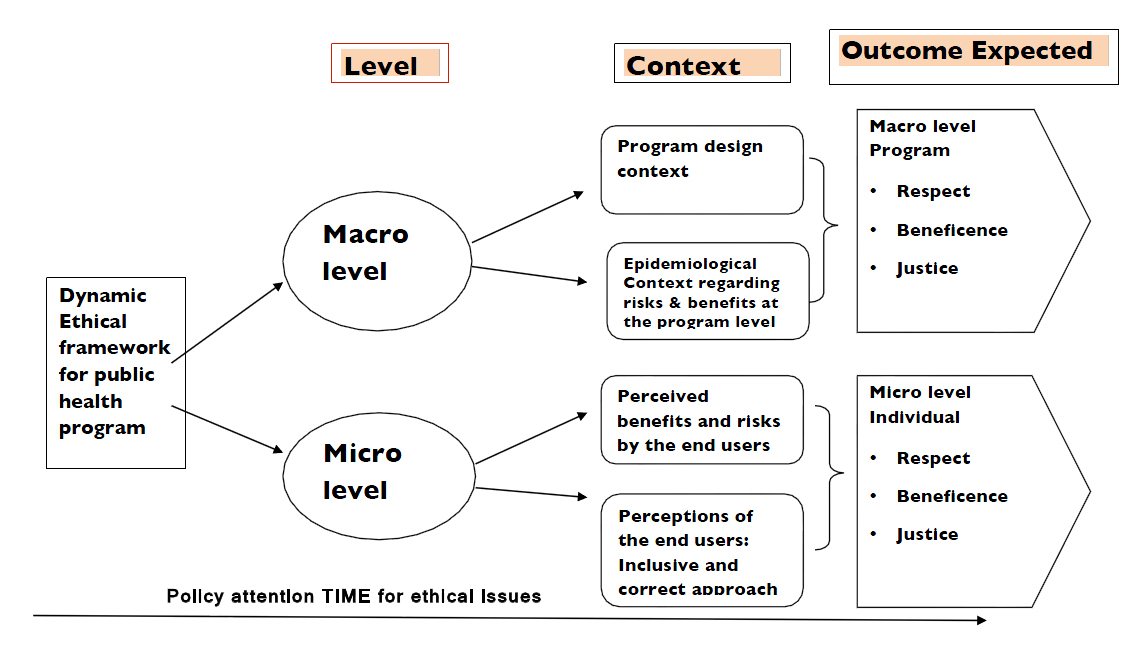
We evaluated the current public health programmes on the basis of the three principles mentioned above. The violation of any of the principles in the framework was seen as a programmatic deficiency or weak point (Figure 1). The principles are outlined briefly below.
Respect for persons (also referred to as autonomy) implies that the choices of autonomous individuals are respected, individuals incapable of making their own choices are protected, and informed decision-making is facilitated through adequate provision of information (7, 8, 9). Respect for persons has also been used in the context of the need to pay attention to the requirements and expectations of communities.
The term justice, in the context of public health programmes, implies that individuals and communities should not be exploited, selection for participation in health programmes must be fair, and vulnerable individuals who may benefit shall not be excluded without good reason (7, 8, 9).
Beneficence (subsuming non-maleficence) mandates that participation in any public health programme should be associated with a favourable risk-benefit ratio. Thus, public health interventions should maximise the possible benefits while minimising potential harm (7, 8, 9).
Results
The RNTCP is the country’s premier vertical programme for the control of tuberculosis (TB). As per the standard definition in infectious epidemiology, the source population for the detection of TB is expected to include all those who are at risk of acquiring TB infection. Hence, the rates of incidence of TB should reflect new infections or new cases of active TB (10). However, according to the earlier definition used by the RNTCP and endorsed by the World Health Organisation (WHO), detection rates should have the number of new “smearpositive” patients detected each year as the numerator, which is operationally convenient and practically feasible (11).
Use of the earlier definition led to an inaccurate estimation of the incidence of TB for the reasons highlighted below. First, it did not include new cases alone, but any case, including prevalent cases (old but not detected). (10) Second, detection rates may not be expected to truly reflect all new cases, since not all patients with new infections or active TB visit a doctor and get diagnosed. In certain regions in low- and middle-income countries, the expectation of a 100% detection rate, predicated on the assumption that all TB-infected individuals would be diagnosed in primary health centres or clinics, is overambitious and, in fact, unrealistic. Third, the fallacious notion that smearpositivity is indispensable to accurate case detection allows smear-negative TB infections to go unrecorded (12, 13). It should also be borne in mind that most widely used diagnostic tests today, such as sputum microscopy, are often not completely effective in the detection of TB.
Thus, though the programme intends to detect the incidence of TB in the country, it is actually determining the prevalence of TB among patients who happen to visit a healthcare centre and test smear-positive. Operational reasons underlie the change of nomenclature whereby prevalence has been termed incidence, and the technical soundness of this definition is a cause for concern. There are several dangers associated with such a change. One, it gives rise to a false sense of complacency that all new cases (incident cases) are being diagnosed, whereas in reality, a significant proportion of the population with new infections is not diagnosed, leading to under-reporting of cases. The current incidence measures depend on several determinants. These determinants are: varying detection rates across different regions/states; varying levels of sputum positivity after detection by clinicians; and different reporting patterns within the same region over a period of time. Further, only the survivors of active/chronic TB figure in each of these estimates, with those who are already dead due to the severity of disease or lack of treatment being left out (14).
TB chemotherapy is intended primarily to decrease the prevalence of the disease (diagnosed and existing cases) rather than its incidence, since it is undertaken subsequent to diagnosis and not vice versa. What would ideally bring down the incidence, which is the stated focus of the RNTCP, are preventive measures rather than therapeutic measures. A few examples of preventive measures are: improvements in lifestyle through programmes aimed at providing well-ventilated housing with adequate space between the units, so that fewer people are compelled to live in crowded settlements; controlling immunodeficiency; and the introduction of effective vaccines, once they are available.
The key underlying ethical issue here is that the basic definition of TB cases hinges around programmatic convenience, geared as it is towards calculating an estimate, and fails to effectively prioritise and address the goal of identifying all TB infections and providing treatment to them. Furthermore, the RNTCP has no focus whatsoever on prevention, a key requirement for reducing the disease burden. It is completely unethical to term prevalence cases as incidence cases, a practice which results in a marginal reduction of TB cases and therefore, allows for the false declaration that the burden of new disease has fallen.
The ethical principle of respect for persons is violated because the public and policy-makers are given either only partial or no information on which to base decisions on whether the programme is truly reducing the incidence of TB or is largely concerned with decreasing the prevalence of TB cases. A detailed paper by Nair in this journal (15) lists several ethical issues concerning the RNTCP. It reports that 90% of patients who suffer from TB are not given any scientific treatment, while 87% of patients who are diagnosed and treated on the basis of an X-ray alone are unlikely to have TB.
All member states of the WHO adopted the goal of detecting at least 70% of all new infectious cases arising each year, and of curing at least 85% of those detected by 2000 (later changed to 2015) (16). The UN Millennium Development Goal (MDG) 6c, related to decreasing the incidence of TB, can be approached in either of the following ways.
- Define cases of TB to actually reflect the entire population that is at risk and determine detection rates on such a definition. This entails improvements in detection and reporting. It is impossible to achieve this without effecting improvements in public health surveillance, and addressing challenges in the management of human resources and infrastructure so as to maximise the reach of the TB programme.
- Continue with the current definition of incidence and conclude that TB is under control. If one adopts the latter approach, one would tend to embrace a more vertical programme at the risk of neglecting the primary health infrastructure as well as the improvement of the health systems (Table 1).
It is possible for low- and middle-income countries to realise the MDG related to the control of TB only if their public health infrastructure undergoes a dramatic improvement. This should ideally be the primary long-term goal not only of programmes aimed at TB control, but also of many other contemporary public health programmes addressing the several health problems plaguing these countries. The use of simple and more practical epidemiological tools can help eliminate the uncertainties in the measurement of the disease burden and its impact on the population, and also, eliminate the false sense of accomplishment, which can lead to complacency (17). It is recommended that population measures of disease, such as incidence and prevalence, be better defined in the context of the implementation of the TB programme. There should also be greater clarity on which aspects of the disease measures are to be addressed. This will help tackle the problem of unjustifiable declarations that there has been a reduction in TB cases.
Drug-resistant forms of TB
Another key issue that the RNTCP aims to deal with is the incidence of drug-resistant forms of TB. The various forms of drug resistance (MDR-TB, XDR-TB and more recently, the socalled XXDR-TB or TDR-TB) have made it more critical than ever to effectively identify, assess and treat incident TB cases so that the incidence of TB can be halted and reversed by 2015, to meet the MDG. By increasing the propensity to cause incident cases of TB, and also increasing the programme’s expenditure on diagnosis and treatment, drug-resistant TB clearly poses a serious obstacle to the complete eradication of TB from the country.
It is important to be aware that the same factors that contribute to the spread of TB and lead to more incident cases also contribute to drug resistance. These include the fact that all patients do not have adequate access to proper treatment. Further, there is a lack of clinical follow-up of patients to ensure adherence to short-course chemotherapy. The poor utilisation and limitations of diagnostic procedures is another factor. Most importantly, there is the issue of the disorganised private healthcare sector, the association of which with the nationallevel public healthcare programme is not supervised or guided in any particular direction (18).
In this context, there is a breach of the ethical principle of beneficence. All the efforts of a public health programme such as the RNTCP would not result in any long-term achievements in disease control and eradication in the absence of better and periodical assessment of the incidence of drug resistance, drastic improvements in the healthcare infrastructure, and a clear foundation upon which to base the implementation of measures that prevent the spread of disease.
The DOTS-Plus programme has been in place as part of the RNTCP since the year 2000, to address some of the issues relating to drug resistance. Its increasing coverage of the disease across the country has led to significant improvements in the rates of the detection of TB (19), However, the programme has not been modified to rectify the prior errors in the management of the disease. Bringing India’s extensive private healthcare sector, which comprises clinicians, private diagnostic facilities and traditional healers, into a single, cohesive public health programme may seem a tough, even impossible, task. However, unless this sector is utilised as a potential resource in a national public health programme such as the RNTCP, and unless guidelines are established to improve the sector’s integration into the programme, little progress can be made in assessing and treating drug-resistant forms of TB across the country. While the RNTCP has made some positive inroads into this area, much more needs to be done by way of providing an integrated and comprehensive response for TB control.
| Table 1
Summary of ethical issues in selected public health programme initiatives in India and their implications at the micro level |
|
| Issues/programmes | RNTCP |
| Respect for persons |
This principle is violated because the public and policy-makers are either not provided any critical information or are provided only some, which makes it difficult for them to make autonomous decisions. False-positive results on X-ray examinations and false-negative results on microscopic examinations go untreated. Not all patients of TB are diagnosed and treated. |
| Beneficence |
Due to the constant emphasis on the treatment of TB, prevention is not considered a priority. The programme does not accurately estimate the true burden of new cases (incidence), but claims that it does. |
| Justice | People who do not have access to the healthcare system do not get a chance to participate in the RNTCP. Given the large population of India, the number of people being neglected by the programme is significant. |
| Summary reflection on ethical perspectives | New definition of incidence needs to be developed. |
| Way ahead to ensure that public health programmes are run ethically to protect beneficiaries and enhance benefits to them | The programme needs to be redefined, with a stronger focus on preventive efforts. Better estimates of incidence rates and periodical monitoring of the trends in treatment will be of use to those designing preventive measures in the Indian context. |
Pointers for the future
The Belmont Report was commissioned in the USA in response to a large number of unethical biomedical research cases, and has greatly influenced the development of the field of biomedical research ethics globally. This is reflected in growing attention in India and other low-and-middle-income countries. Due to a variety of factors, ethical concerns in public health programmes often do not receive the same extent of coverage as the ethical aspects of biomedical research/clinical trials. First, public health programmes are rarely required to obtain ethical clearance before their implementation, particularly in low- and middle-income countries. Second, there are only a few ethical frameworks that have been specifically developed for application to public health programmes, and these are not widely known. Third, there is a perception among the health managers that they are doing the public good by implementing the public health programme and hence, minor aberrations or side-effects that affect a few individuals are tolerable (if not justified). That they harbour good intentions towards the public is mistaken for being ethical, and in many cases, programme managers do not even examine whether there is a need for ethical review and monitoring. This article has attempted to draw attention to examples of violations of the ethical principles of respect for persons, beneficence and justice. At times, proactive measures need to be taken in research, in preference to reactive measures to gross violations. We hypothesise that using pre-emptive ethical screening for the development and implementation of health programmes might help to limit possible violations.
|
Table 2 Ways of implementing ethical principles in public health practice at the macro level |
||||
| Macro level determinants | Ethical principle | Goal to be reached | How to implement it in public health practice | |
| 1 | Autonomy | Enhancing public understanding and trust in public health programmes |
|
|
| 2 | Beneficence | Favourable risk-benefit ratio |
|
|
| 3 | Justice | Equitable participation |
|
|
The implementation of any new public health programme should be guided by consultations with ethicists, public health consultants, scientific organisations and the general public. The programme should be discussed by various stakeholders, including the people’s representatives in the media and forums for generating awareness among the people. There should be standard operating procedures (SOPs) for seeking ethical approval for new programmes. The SOPs should focus on improving the quality of services, monitoring the adverse effects of the programme, maintaining a registry of grievances, supporting people affected by adverse effects, and addressing misconceptions about the programme. As a first step, the existing public health programmes can be reviewed on the basis of this framework (Table 2).
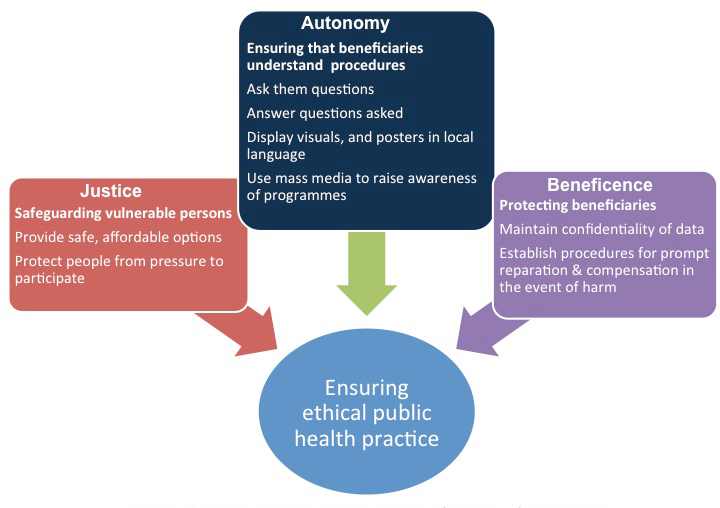
An example of an ethical framework within which a public health programme should function is illustrated in Figure 2. We stress the need to bring the science of public health to the level of lay persons so that they understand it well enough to make decisions, at an individual, family and community level, about whether or not to avail themselves of public health services. One of the important challenges to the implementation of ethical frameworks is the mindset of health managers and those who make policies on healthcare. Currently, in low- and middle-income countries, those framing health policies often assume the role of decision-makers on behalf of the people (“for their good”). We argue that where possible, concerted efforts should be made to encourage decision-making (with respect to accepting or rejecting public health interventions) at the individual and community level by the people themselves, and health managers should facilitate this. We believe that implementing ethical frameworks would make the focus of public health programmes more “user-friendly”, rather than “management-friendly”, as they are at present.
Conclusions
In this paper, we have examined the applicability of the principles of respect for persons, beneficence and justice to the implementation of the TB control programme in India. We applied these principles, which have primarily been used as a framework for evaluating research on human participants, in the context of public health policy and programme implementation in the country (Figure 2).
Numerous ethical dilemmas must be confronted in the area of public health practice in the modern world (14, 20). Governments and international agencies are sometimes successful in addressing these dilemmas during the implementation of public health programmes. However, we argue that most ethical violations may be prevented if ethical frameworks are adopted before implementation. We propose the application of one such framework, consisting of the principles of respect for persons, beneficence and justice, as adapted to public health practice, to serve as an ethical guide in the implementation of public health programmes. These principles should be shared with policy-makers and used during decision-making in public health programmes. We have presented an ethical evaluation of the TB control programme in India as an example. Similarly, an ethical evaluation of all the proposed and ongoing public health programmes at the national and international levels can make an incremental positive difference in the lives of the people.
References
- Roberts MJ, Reich MR. Ethical analysis in public health. Lancet. 2002 Mar 23;359(9311):1055-9.
- Hodge JG, Jr, Gostin LO. Public health practice vs. research: A report for public health practitioners including cases and guidance for making distinctions [Internet]. Atlanta, GA:Council of State and Territorial Epidemiologists; 2004 [cited 2013 Nov 18]. Available from: http://www.publichealthlaw.net/Research/Affprojects.htm#CSTE
- Dye C, Bassili A, Bierrenbach AL, Broekmans JF, Chadha VK, Glaziou P, Gopi PG, Hosseini M, Kim SJ, Manissero D, Onozaki I, Rieder HL, Scheele S, van Leth F, van der Werf M, Williams BG. Measuring tuberculosis burden, trends, and the impact of control programmes. Lancet Infect Dis. 2008;8(4):233-43. doi: 10.1016/S1473-3099(07)70291-8. Epub 2008 Jan 16
- Dye C, Maher D, Weil D, Espinal M, Raviglione M. Targets for global tuberculosis control. Int J Tuberc Lung Dis 2006 Apr;10(4):460-2.
- Centers for Disease Control and Prevention, US Department of Health and Human Affairs. Recommendations of the International Task Force for Disease Eradication [Internet]. Morbidity and Mortality Weely Report. 1993[cited 2013 Nov 18];42(No. RR-16):1-38. Available from: http://www.cdc.gov/mmwr/PDF/rr/rr4216.pdf
- Nelson-Rees WA. Responsibility for truth in research. Philos Trans R Soc Lond B Biol Sci. 2001;356(1410):849-51.
- World Medical Association (WMA) Declaration of Helsinki. Ethical principles for medical research involving human subjects. Adopted by the 18th World Medical Association General Assembly, Helsinki, Finland, June 1964.
- The National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research. The Belmont report. Ethical principles and guidelines for the protection of human subjects of research. Washington, DC: Department of Health, Education, and Welfare; April 18, 1979.
- Council for International Organizations of Medical Sciences. International ethical guidelines for biomedical research involving human subjects. Bull Med Ethics. 2002 Oct;182:17-23.
- Rothman KJ, Greenland S, Lash TL. Modern epidemiology, 3rd edition. Philladelphia, PA: Lippincott Williams & Wilkins; 2008.
- Chauhan LS, Agarwal SP. The Revised National Tuberculosis Control Programme. In: Chauhan LS, Agarwal SP, editors. Tuberculosis control in India. New Delhi: Directorate General of Health Services, Ministry of Health and FamilyWelfare; 2005, pp. 23-34.
- Begum V, Van Der Werf MJ, BecxBleumink M, Borgdorff MW. Viewpoint: do we have enough data to estimate the current burden of tuberculosis? The example of Bangladesh. Trop Med Int Health. 2007;12(3):317-22.
- Van Der Werf MJ, Borgdorff MW. How to measure the prevalence of tuberculosis in a population. Trop Med Int Health. 2007;12(4):475-84.
- Attaran A. An immeasurable crisis? A criticism of the millennium development goals and why they cannot be measured. PLoS Medicine. 2005;2(10):e318. doi: 10.1371/journal.pmed.0020318
- Porter J, Ogden JA. Ethics of directly observed therapy for the control of infectious diseases. Bulletin de l’Institut Pasteur. 1997;95(3):117-27.
- World Health Organization. Forty-fourth World Health Assembly. Resolutions and Decisions. Resolution WHA 44.8[Internet]. Geneva:WHO;1991[cited 2013 Nov 18]. Available from: http://www.who.int/bulletin/volumes/87/12/09-070169/en/
- Babu GR. Comment on ‘From risk factors to explanation in public health’. J Public Health. 2008;30(4):515-16.
- Babu GR, Laxminarayan R. The unsurprising story of MDR-TB resistance in India. Tuberculosis (Edinb). 2012 Jul;92(4):301-6. doi: 10.1016/j. tube.2012.02.009
- Empowered Procurement Wing, Ministry of Health and Family Welfare. Government of India. RNTCP Launches Cat IV (DOTS Plus) treatment for Multi-Drug Resistant TB [Tuberculosis Control Program][Internet]. New Delhi: Government of India 2013 [updated June 26 2013][cited 2013 Nov 20]. Available from: http://mohfw-epw.gov.in/index.php?option=com_content&view=article&id=68:rntcp-launches-cat-iv-dots-plustreatment-for-multi-drug-resistant-tb&catid=46:facts-a-figures
- Detels R. Epidemiology: the foundation of public health. In: Detels R, McEwen J, Beaglehole R, Tanaka H, editors. Oxford textbook of public health. Oxford and New York: Oxford University Press; 1999, pp. 485-91.