ARTICLES
How ‘informed’ is informed consent? Findings from a study in South India
Shuba Kumar, Rani Mohanraj, Anuradha Rose, MJ Paul, George Thomas
DOI: https://doi.org/10.20529/IJME.2012.061
Abstract
A qualitative study using in-depth interviews was carried out among patients and doctors working in a private hospital in Tamil Nadu, to understand perceptions of informed consent. Audio-recorded interviews were transcribed verbatim and a framework analytical approach was used in analysis. Emergent themes ranged from perceptions on informed consent, and discussing health concerns and decision making, to information provided by and expectations from doctors, and suggestions for improvement. Most patients were unfamiliar with the kind of information provided in the informed consent process; a few felt that the information was inadequate. Decision making about surgery was left mostly to the doctor. Poor literacy in patients was seen as a barrier to effective communication by doctors. Developing local language versions of consent forms supported by audiovisual aids is needed for patients to take a proactive role in their treatment process, and for doctors to be receptive to patients’ needs and capacities.
Introduction
Informed consent has increasingly become a major topic of discussion and debate. While the need for client participation in healthcare decision making has been acknowledged, its implementation has been varied and individualistic. Haas (1) says that while some variations in this process are appropriate as circumstances can differ, others result both from confusion about these issues and passive resistance to new demands. Although the informed consent process is followed in most medical settings, evidence of patients’ experiences of the consent process remains limited.
Studies from developing countries show that patients view written consent as ritualistic and bureaucratic. Some feel frightened or pressured to give consent (2, 3). According to Moazam (4), the unquestioned authority of the medical profession and a fatalistic belief among the population about illness and death leave patients open to exploitation. She identifies a lack of awareness of individual rights and redress through the judicial system, which is not easily accessible. Consequently, the risk of exploitation of patients by healthcare professionals is real. Perez-Moreno (5) analyses the quality of information provided prior to anesthaesia and surgery in 300 patients and found that a majority of patients had poor knowledge of surgical and anaesthetic risks. Concerns regarding erosion of patient autonomy and subordination of patients’ interests to the competing interests of the family also exist, particularly in paternalistic societies (6).
The above scenario is similar in India. Typically, the oldest male member in the family makes major decisions. Where women patients are concerned, the complex patriarchal nature of the structure of Indian society in turn dictates the nature of this relationship between the doctor and the female patient, with women often expected to be acquiescent, allowing the senior family member to do the talking (7). Furthermore, patients generally tend to put the onus of care on the doctor. This attitude is typical of most Eastern religions which view the art of healing as ‘work most worthy of men’ (8). Focshen et al (7) report that doctors tend to view patients’ knowledge as ‘not worth taking into consideration’. They further state that as patients are seen as lacking in capacity to fully understand the information provided, trying to communicate to them is often seen as a futile exercise.
Considering the above, researchers in India are beginning to recognise the limitations of standard informed consent forms. For non-literate and semi-literate persons, this document is viewed with suspicion and one to which they are reluctant to affix their signatures or thumb impressions. In other instances, the informed consent process has become a mere formality with subjects/patients simply acquiescing to whatever is required of them. Given the above, informed consent that hinges purely on the principle of autonomy and rational decision making as understood in the West is problematic. With this background, we carried out a qualitative study among patients and healthcare professionals working in a private hospital in the southern state of Tamil Nadu, India, to understand the process of informed consent as it operated there. Specifically, the study sought to ascertain how patients and healthcare professionals perceived informed consent and the constraints to obtaining informed consent, and what their suggestions were on improvements.
Methods
A cross sectional study using in-depth interviews was carried out in the department of surgery of a large private tertiary level hospital in southern Tamil Nadu. Ethical clearance was obtained from the Institutional Review Board (IRB) of the hospital. Using purposive sampling, consenting Tamil speaking adult patients admitted to undergo surgery and doctors working in the department of surgery were included. Patients were approached following completion of their surgery. Only those who were physically fit enough to participate in the interview and gave written consent were included. All interviews were carried out in privacy and both patients and doctors were assured of confidentiality. Separate in-depth interview guides for patients and doctors were developed. Efforts were also made to explicitly solicit suggestions on improvement of the consent process. The guide for patients sought to elicit details on patients’ perceptions of the meaning of informed consent, information communicated to patients, and the comfort level of patients in asking questions to the doctor. The guide for doctors included issues such as how they understood informed consent, description of the informed consent process currently underway in the hospital, their satisfaction/dissatisfaction with it, perceptions on the nature and quantum of information to be provided to a patient, and constraints to obtaining informed consent in the hospital setting
Analysis
All interviews were audio recorded, and transcribed verbatim. Those carried out in Tamil were first transcribed verbatim and then translated into English, to allow for analysis using a qualitative software. A framework analytical approach was used for data analysis (9). This process, involving a number of highly interconnected and iterative stages, began with data immersion. This was followed by a series of other stages involving identifying a thematic framework: sifting through the data, identifying meaningful and relevant quotes; placing the quotes under the appropriate thematic category; mapping; and finally interpretation. Each transcript was coded inductively by two independent researchers (SK and RM). After coding 3 interviews, the coders compared the coding schemes each had developed, resolved any differences in coding and developed a common coding framework that was used to code all other interview transcripts. Once all the interviews were coded, segments of text that were related to a common theme were pieced together and in this manner emergent themes were identified. The qualitative analysis was done using NVIVO.
Results
Demographic characteristics
A total of 14 patients (8 women, 6 men) aged 25 years and above were interviewed. All were from Tamil Nadu and hence all interviews were carried out in Tamil. Three men and one woman had completed graduation, 5 had completed 10-12 years of schooling (secondary school) and 4 had completed 5-6 years of schooling (primary school). All the patients were married barring two women who were unmarried. The surgical procedures that these patients underwent ranged from appendicitis, hydrocele, fibroids, and toe amputation to caesarean section and colostomy. A total of 8 doctors (2 women, 6 men) were interviewed, 2 of whom were heads of their departments aged 50 years or more, while the remaining 6 were junior and senior residents aged between 22 and 30 years.
Themes of analysis
The themes that emerged were:
- Perceptions of informed consent
- Information provided by healthcare providers to patients
- Perceptions on discussing health concerns and decision making
- Expectations from the healthcare facility/providers
- Suggestions for improving consent procedures
(see Table : Quotes from interviews)
Perceptions on informed consent
For many patients, “informed consent” was an unfamiliar phrase. They did not know what it meant aside from having to sign a form, the contents of which were only vaguely known to them. One young woman patient said that she had never paid any attention to these issues and had left it entirely to her mother. To others, it implied a document by which the hospital could protect itself in the event of any mishap. Others understood that it entailed a process whereby doctors communicated details about the nature of surgery that was to be performed, and advised them of potential risks and benefits. Some educated patients believed that non-literate patients were at a disadvantage as they understood little and the onus was on doctors to help them understand.
Doctors, for the most part, were familiar with the concept of informed consent. Issues concerning ethics and informed consent were taught to them as part of their medical curriculum. Although most were unable to clearly name the three broad principles of ethics (respect for persons, beneficence and justice), they were, able to provide fairly clear explanations of what informed consent entailed. One doctor spoke of the importance of giving patients the right to decide and making the effort to explain to patients in a manner that would help them understand. A few doctors held different positions and felt it was alright for doctors to take the lead and make the decisions considering their expertise and experience in the field.
Information provided by healthcare providers to patients
In terms of content, most patients said that doctors had described the specific surgical procedure in fair detail. This happened over several sittings beginning with the first visit which was in the outpatient’s department. Many times, this explanation was done with the help of a sketch to demonstrate what the surgery entailed. According to the patients, doctors also told them about potential risks but generally softened this by saying that “everything would be alright”. In contrast, a few patients said that not much information had been given to them, and what little they had gleaned was by overhearing conversations between medical personnel. One woman who had recently undergone a caesarean section said that neither doctors nor nurses had prepared her for the possibility of caesarean section. Nor had they apprised her, during her antenatal consultations, of the aftereffects of having such a surgery. While underscoring the importance of doctors communicating clearly to patients, the need for patients to play a proactive role in the treatment process was also highlighted. However, patients reported varied reactions to the information provided by doctors regarding their illness and treatment, which ranged from appreciation to feeling overwhelmed and afraid.
Table : Quotes from interviews
Perceptions on informed consent
“I asked whether I should sign the form or my husband shouldsign the form and they told me that if I sign the form it is okay.But I don’t know for what reason they got the signature.”
(Female, 43, primary school educated).
“At the time of surgery if something happens, like if they dothe surgery on the wrong side, we cannot question them. Thatis what I have read in the form.”
(Male, 27, college educated).
“Initially I never even thought of it (informed consent). As longas we are not harming people and are doing things to helpsociety, it was not even important for me. But after I startedgetting involved in research, I began to learn more about it. Ibecame convinced that it is an important aspect.”
(Doctor, male, 50).
“This (ethics) is something instilled in us when we study here.”
(Doctor, male, 24).
Perceptions on discussing health concerns and decision making
“It is like talking back to the doctor. The doctors come andexamine discuss among themselves and decide. What is therefor me to ask the doctor?”
(Male, 62, college educated).
“For everybody life is very important and people are scared toask questions to the doctor for fear that the doctor will eithernot treat them or else not give them the correct treatment.”
(Male, 25, college educated).
“When we see a patient we always see them with a relative, soinformation goes to both the patient and the relative. Time isalways taken to explain to them what is wrong with the patientand what needs to be done.”
(Doctor, male, 27).
“I think it is ok for doctors to decide, after all we are the oneswho understand the pros and cons so it is obvious that weshould be the ones making the choices. I don’t think it is fair toask the patient to decide. It is like buying software. If you ask meto go and buy one, I really know nothing about it. Even if youtold me that this software has these features etc I would still beclueless at the end of it and will depend on the computer expertto guide me. So I feel somewhat the same. We have been inthis field of medicine for (years)and our understanding is alsodifferent (from that of a non-medical person). We cannot expecta non-medical person to have that same understanding.”
(Doctor, male, 53).
Information provided by healthcare provider topatients
“On many occasions when we try to explain things or tell them(patients) why we are doing a certain procedure, they say it doesn’t matter and that they don’t really want to know. Theysay, ‘If you say it has to be done, then I will do it.’ ”
(Doctor, male, 50)
“I keep the patient informed, if they (relatives) don’t want meto tell the patient, then I will not tell them what the diseaseis, but I will tell (the patient) everything else. But I do tell thefamily members that within 48 hours they need to informthe patient and that if they do not do so I will. Before theoperation we make sure that the patient knows the diagnosisand the likely outcome.”
(Doctor, male, 55)
“Some patients find it difficult to understand the concepts.For them we draw and show them; I simplify it so they canunderstand. We have a generic form which is applicable for allkinds of operations but issues like the risks, complications wehave to write and fill in the form.”
(Doctor, female, 22)
“I feel in our country the burden on the doctor is much morethan in other countries. Here quite often the doctor is forcedto decide for the patient. Many patients do not have theknowledge and they will tell us, ‘You tell me what is the rightthing to do.’ Most of the time they (patients) don’t even knowwhat procedure they have undergone. They don’t know aboutcomplications, they don’t even know the diagnosis. Sometimesit can be extremely difficult.”
(Doctor, female, 30)
Expectations from the healthcare facility/provider
“The doctor did not give any instructions on what I need to doto take care of myself after a caesarean. They need to give meall this information at the outset.”
(Female, 37, secondary school educated)
“The doctor has to spend time with the patient. If the doctorcomes just for a few minutes and walks away, you don’t feel likeasking him any doubts freely because he will not be in a moodto listen to you and hear what you are saying.”
(Female, 43, primary school educated)
Suggestions for improving consent procedures
“I believe that the doctor knows what is the best thing to bedone, but the patient should ask the doctor his doubts. Heshould ask for all information about his operation.”
(Female, 36, primary school educated)
“Social workers will need to be properly trained as this(medicine) is a highly specialised field and they should be ableto communicate clearly to patients … It may take a long time totrain them but then they can be very helpful to us and may helpto decrease the workload of doctors.”
(Doctor, female, 30)
The doctors explained that in almost all cases patients were seen along with a family member and details concerning the illness/surgery were jointly explained to both. The consent form used in their facility was described as a two-part document comprising information and consent. The information section was usually written up in brief by the doctor. The consent section was usually a standard printed form, which the patient was asked to sign indicating acceptance to undergo the surgery. Consent was obtained on the day of the surgery. Sometimes, at the behest of relatives, doctors would refrain from giving details to the patients but they would insist that patients needed to be apprised of risks and complications at some point before surgery. This need to inform patients about potential risks and benefits irrespective of what relatives thought was underscored by all the doctors.
Perceptions on discussing health concerns and decision making
Patients gave various reasons for not asking questions to their treating doctors. The most common reason hinged on their deep sense of faith and trust in the specific hospital or doctor and the conviction that the ‘doctor knows best’. Another concern was that of appearing poorly in the eyes of the doctor if they were to ask a lot of questions. The perception that raising questions would be seen as being rude, coupled with the fear of annoying the doctor who then may not deliver proper care, was often reported. Others believed that it was the duty of the doctor to provide all the necessary information to the patient without the patient even having to ask for it. Decision making about surgical procedures, too, was largely left to the doctor although patients did discuss it with their families. However, they depended on their doctors to guide them.
The total dependence and faith that patients reposed in doctors, coupled with reluctance on the part of many patients to learn more about their health condition, often prompted doctors into communicating minimally to patients and making decisions for them. Some doctors spoke of the dynamics of the doctor-patient relationship that seemed to suggest that the doctor was on a higher plane when compared to the patient and thereby more empowered to make these decisions. A few doctors spoke of the limited ability of patients to understand issues concerning their illness as well as complications related to the surgery, which they perceived as a deterrent to the process of informed consent. Despite this, doctors believed that patients needed to be involved in and apprised of the facts of their surgical procedure. In a few instances, doctors spoke of language as a barrier to effective communication. All doctors reiterated that the operating doctor by virtue of his/her primary responsibility to the patient went through the consent process, but obtaining the signature on the consent form was delegated to a junior doctor.
Patient expectations from the healthcare facility/providers
One of the most consistent expectations repeated by patients was that doctors needed to spend time and explain their illness/surgery in a manner that they would understand. The importance of describing what sort of post-operative care needed to be taken was also stressed. Others spoke of the value of using flip charts, sketches or other visual aids to help explain surgical procedures in a simple and effective manner but also felt that this needed to be used with caution as it could frighten patients. Most patients saw the doctor as the ideal person for obtaining consent; only two felt that anyone of the medical staff would be acceptable.
Doctors’ perceptions on improving informed consent processes
Suggestions given by doctors ranged from developing language versions of consent forms and getting social workers to obtain consent to relieve the burden on doctors, to developing audiovisual aids – either in the form of flip charts or as material downloaded from the internet. Some said that the inability to read on the part of many patients tended to preclude the usefulness of language forms. Having social workers talk to patients and explain details about their illness and surgery was appreciated by most doctors but they underscored the importance of making sure these social workers were well trained, and professional in the manner in which they obtained consent.
Discussion
Culture and informed consent
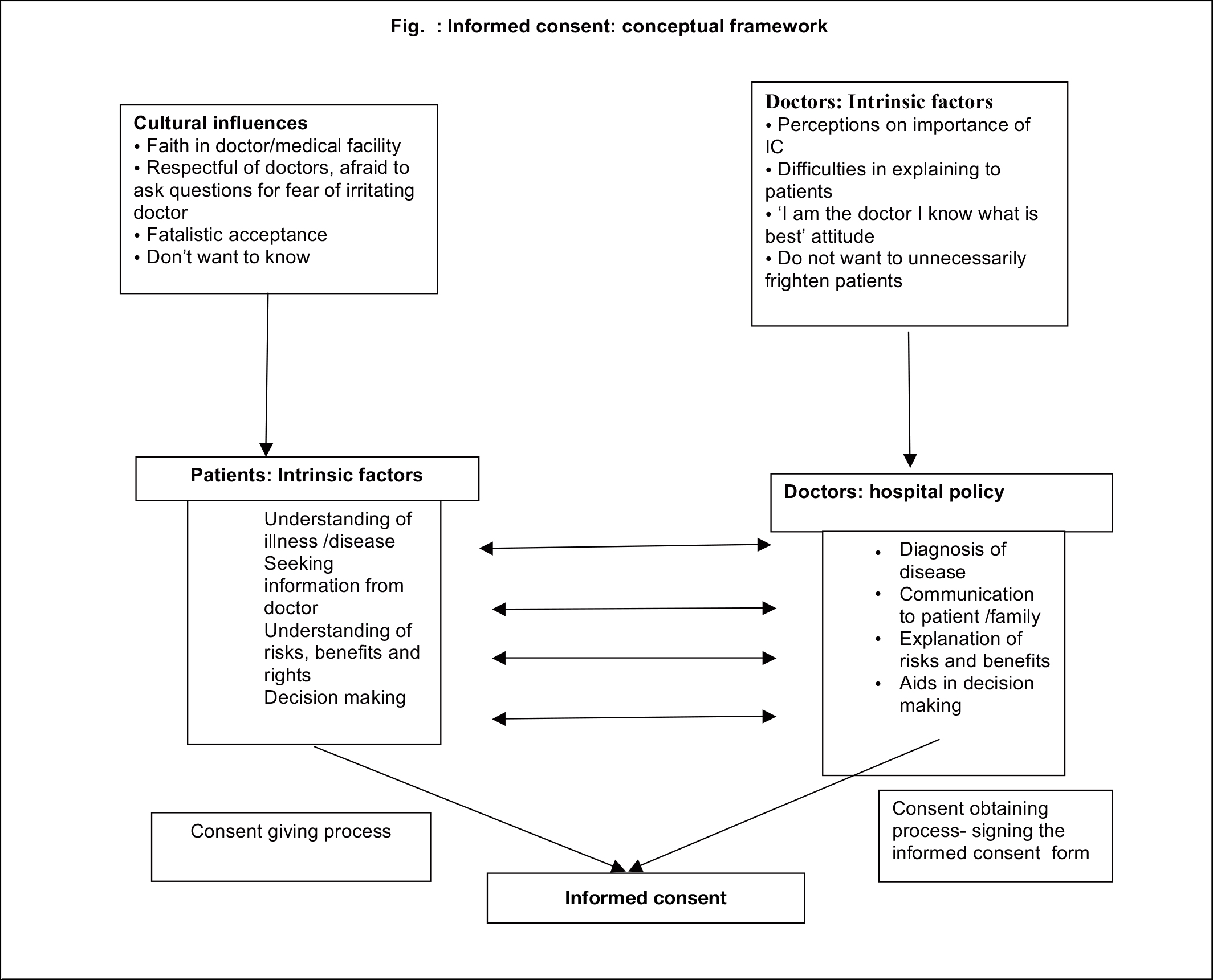
The findings from this study revealed that an understanding of informed consent among the study participants could at best be termed moderate, but was for the most part inadequate. Implicit faith combined with a deep and abiding respect for doctors and the fear that asking questions to the doctor would be seen as rude behaviour acted as deterrents to patient participation. These cultural influences cut across different sections of society and being educated did not imply being proactive. Interestingly, this implicit faith in the medical profession (Fig.) is observed in most societies (4, 10, 11). Doctors, for the most part, believed in communicating key issues to patients but often found poor literacy levels and language barriers prevented effective communication. Studies carried out in western countries have also shown that patients’ understanding of their health condition, prognosis, treatment and the risks involved were not complete owing to their cognitive and emotional limitations (11, 13). Some doctors in our study believed that they should advise patients on what choices to make because of their expertise and experience. While it is true that the consent process is all about providing adequate information to patients so that they can make these choices, those with poor literacy often tend to feel overwhelmed and unable to make these decisions and preferred leaving it to the doctor. A study carried out by Fink et al (14) demonstrated that patients who were elderly, belonged to the African-American or Hispanic races, with less than high school education, experienced difficulty in comprehending the details of their surgical procedure. However, the use of adjuncts like ‘repeat back’ (patients are asked to state in their own words whatever they have understood from what was read out to them through the consent form) improved patient comprehension significantly. Krankl et al (15) too concluded that greater attention needed to be given to patients’ educational background to ensure adequate understanding of clinical information. In this context, Bernat and Peterson (16) have reported on the value of doctors developing a good understanding of exactly what and how to communicate to help patients understand better. These proactive steps by doctors combined with building awareness about these processes among patients could aid in making informed consent ‘truly’ a two-way process rather than the one-sided one that it currently is.
The informed consent form
The perception that the consent form was a defensive tool used to protect doctors/hospitals was reported by patients and their families. This was reported by Akkad et al (17) in a study from England. Further, there was considerable uncertainty among patients about the implications of signing/not signing the consent form. In our study too, the fact that only a few patients spoke of the consent form as a document that was in their interest was disquieting, as it implied poor understanding about the true purpose of the consent process. The clear guidelines about the depth and detail required in the consent form in research are not reflected in the clinical field. Information about the surgery was written down, sometimes briefly, sometimes combined with sketches by the doctor, allowing a considerable amount of variability in terms of what was actually described. The consent form that was used consisted of a printed form outlining that the patient was aware of the potential risks and had consented to surgery.
The meaningfulness of the written consent form has been debated widely. Studies have shown that many patients do not read the consent form, primarily because of their preference for verbal information (3, 18). Many also find it hard to understand. Most patients in India do not read the form because of poor literacy. But more typically, it could be attributable to the belief that the ‘doctor knows best and will not deliberately harm me.’ However, the use of visual aids like drawings and sketches during consultations prior to surgery were found by patients to be helpful. Research has shown that the use of decision aids and supplementary educational material during the informed consent processes improves patients’ comprehension and is associated with patients’ increased knowledge about their condition, low decisional conflicts and reduced use of elective procedures (19, 20, 21, 22). Perhaps, the use of more structured visual aids (flip charts, videos) could help patients understand better, and instil the purpose and value behind getting involved in their recovery process. This could be the way to go forward in the future.
Who should obtain consent?
The question of who should obtain consent received a near unanimous response. Most patients believed that their doctor was the right person to take them through the consent process and most doctors agreed with this view. Although it is true that the consent process usually happens over several sessions, the fact remains that most doctors work in very busy clinics and quite often are not able to spend time with patients. For patients, the need to emotionally connect with doctors, gain their reassurance and have the doctor ‘come down to their level’ and explain the pros and cons in a less hurried atmosphere is critical. Sanyal et al (23) reported that Indian patients are able to comprehend and should be informed about the details of their operation but highlighted that the informed consent process should be a continuous one rather than a single event. Physicians at the Temple University in the US identified several challenges in direct relation to informed consent based on a review of patient-doctor communications (24). Many of these, like lack of clinician time, poor patient literacy, and language and cultural issues, were cited by both the patients and physicians in our study, which in turn suggests the need for the development of consent guidelines that are more in keeping with what patients want.
A limitation of our study was that we did not include a government hospital or even another private hospital as a comparison. The selected hospital by virtue of its strong service-oriented philosophy cannot be considered reflective of the situation that prevails in other hospitals. However, the strength of the study lies in the use of qualitative methods, which allowed patients and doctors to speak freely, thereby lending credibility to the findings.
Conclusion
The doctor-patient interaction has been widely acknowledged as an important factor influencing patient health outcomes (25). Given this, it is imperative that the one-sided doctor-dominated relationship gives way to a more patient-centric approach (26). The study findings highlight the need for patients to take a proactive role in their treatment process, and for doctors to be receptive to patient needs and capacities, and provide information that can be easily understood. Such a participatory relationship where treatment decisions are made in an environment where patients feel free to air their concerns, and where doctors understand and respect these concerns, would be the most appropriate strategy towards obtaining ‘truly’ informed consent. This, combined with the use of more structured visual aids could help patients better understand the medical/surgical procedures they are about to undergo. Perhaps, this would help set the stage for the development of consent guidelines and strategies that are culturally appropriate and reflect patient needs. As rightly argued by Doyal (27), despite the potential limitations that patients may have in understanding clinical information, the onus is on healthcare providers to improve their methods of communication, even to the extent of taking recourse to better educational aids as a means of facilitating the informed consent process and ensuring better understanding by patients.
References
- Haas LJ. Hide-and-seek or show-and-tell? Emerging issues of informed consent. Ethics Behav. 1991;1(3):175-89.
- Habiba M, Jackson C, Akkad A, Kenyon S, Dixon-Woods M. Women’s’ accounts of consent to surgery: qualitative study. Qual Saf Health Care. 2004;13:422-7.
- Akkad A, Jackson C, Dixon-Woods M, Kenyon S, Taub N, Habiba M. Informed consent for elective and emergency surgery in obstetrics and gynecology: a questionnaire study. BJOG. 2004;111:1133-8.
- Moazam F. Families, patients, and physicians in medical decision making: A Pakistani perspective. Hastings Cent Rep. 2000;30:28-37.
- Perez-Moreno JA, Perez-Carceles MD, Osuna E, Luna A. Preoperative information and informed consent in surgically treated patients. Rev Esp Anestesiol Reanim. 1998;45:130-5.
- Blustein J. The family in medical decision making. Hastings Cent Rep.1993;23:6-13.
- Fochsen G, Deshpande K, Thorson A. Power imbalance and consumerism in the doctor-patient relationship: Health care providers’ experiences of patient encounters in a rural district in India. Qual Health Res. 2006;16:1236.
- Scully C, Wilson N. Culturally sensitive oral health care. London: Quintessence Publishing Company Ltd;2006. 183p.
- Ritchie J, Spencer L. Qualitative data analysis for applied policy research. In: Bryman A, Burgess RG, editors. Analysing qualitative data. London: Routledge;1994. p 173-94.
- Fetters M. The family in medical decision making: Japanese perspectives. J Clin Ethics. 1998;9:132-46.
- Rogers AE, Addington-Hall JM, Abery AJ, McCoy AS, Bulpitt C, Coats AJ, Gibbs JS. Knowledge and communication difficulties for patients with chronic heart failure: qualitative study. BMJ. 2000;321:605-7.
- Sutherlund H, Lockwood G, Till J. Are we getting informed consent from patients with cancer? J R Soc Med. 1990;83:439-43.
- Lloyd A. The extent of patients’ understanding of the risk of treatments. Qual Healthc 2001;10(Suppl I):i14 – 13.
- Fink AS, Prochazka AV, Henderson WG, Bartenfeld D, Nyirenda C, Webb A, Berger DH, Itani K, Whitehill T, Edwards J, Wilson M, Karsonovich C, Parmelee P. Predictors of comprehension during surgical informed consent. J Am Coll Surg 2010 Jun;210(6):919-26.
- Krankl JT, Shaykevich S, Lipsitz S, Lehmann LS. Patient predictors of colposcopy comprehension of consent among English- and Spanish-speaking women. Women’s Health Issues. 2011 Jan-Feb;21(1):80-5. Epub 2010 Sep 15.
- Bernat JL, Lynn PM. Patient centered informed consent in surgical practice. Arch. Surgery. 2006;141:86-92.
- Akkad A, Jackson C, Sara K, Dixon-Woods M, Taub N, Habiba M. Patients’ perception of written consent: questionnaire study. BMJ.2006 Sep 9;333(7567):528. doi:10.1136/bmj.38922.516204.55
- Agard A, Hermeren G, Herlitz J. Patient’s experience of intervention trials on the treatment of myocardial infarction: Is it time to adjust the informed consent procedure to the patient’s capacity? Heart.2001;86:632-7.
- Schenker Y, Fernandez A, Sudore R, Schillinger D. Interventions to improve patient comprehension in informed consent for medical and surgical procedures: a systematic review. Med Decis Making. 2011 Jan-Feb;31(1):151-73. Epub 2010 Mar 31.
- Volk RJ, Hawley ST, Kneuper S, Holden EW, Stroud LA, Cooper CP, Berkowitz JM, Scholl LE, Saraykar SS, Pavlik VN. Trials of decision aids for prostate cancer screening: a systematic review. Am J Prev Med. 2007 Nov;33(5):428-34.
- Whelan T, Levine M, Willan A, Gafni A, Sanders K, Mirsky D, Chambers S, O’Brien MA, Reid S, Dubois S. Effect of a decision aid on knowledge and treatment decision making for breast cancer surgery: a randomized trial. JAMA. 2004;292:435-41.
- O’Connor AM, Bennett CL, Stacey D, Barry M, Col NF, Eden KB, Entwistle VA, Fiset V, Holmes-Rovner M, Khangura S, Llewellyn-Thomas H, Rovner D. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2009:CD001431.
- Sanwal AK, Kumar S, Sahni P, Nundy S. Informed consent in Indian patients. J R Soc Med. 1996 Apr;89:196-8.
- Bury M. Researching patient-professional interactions. J Health Serv Res Policy. 2004;9:48-54.
- Kaba R, Sooriakumaran P. The evolution of the doctor-patient relationship. Int J Surg.2007;5:57-65.
- Travaline JM, Ruchinskas R, D’Alonzo GE. Patient-physician communication: why and how. J Am Osteopath Assoc. 2005 Jan;105(1):13-8.
- Doyal L. Informed consent: moral necessity or illusion? Qual Healthc. 2001;10(Suppl I):i29 – i3.