ARTICLES
Awareness of medical ethics among undergraduates in a West Bengal medical college
Biswajit Chatterjee, Jhuma Sarkar
DOI: https://doi.org/10.20529/IJME.2012.029
Abstract
This descriptive, cross-sectional study was conducted to assess the knowledge of and attitudes towards medical ethics among undergraduate medical students. It also looked at whether there was any improvement with additional years of medical education. 340 medical students of a medical college in West Bengal were given a semi-structured questionnaire that included questions regarding their awareness of ethics, their attitudes towards various issues in clinical ethics, and their knowledge of the code of medical ethics of the West Bengal Medical Council. The responses of 322 students were analysed by simple descriptive statistics.
The students generally agreed that awareness of ethics was important. Lectures (54.7%) and books (47.8%) were their predominant sources of knowledge. Only 10.9 % were aware of the existence of an institutional ethics committee and 42.8% did not know its exact role. Their answers showed that the majority of students expressed mixed responses – both desirable and undesirable – in relation to questions exploring different aspects of basic ethical reasoning in their professional life. The most desirable response for each statement was decided by experts of forensic medicine and also from a literature study. Only half the respondents (50.9%) had a good score (61-70 out of a total possible 90) and 37.2% had a fair score (51-60). There was no increase in scores corresponding with additional years of medical education.
Introduction
Medical practice throughout the world has become increasingly commercialised, and ethics has taken a backseat. Ethics teaching has been shown to have a significant influence on the professionalism and moral qualities of medical professionals (1, 3). Various methodologies have been tried to stimulate better ethical conduct in health professionals, such as lectures, seminars, interactive workshops, and case conferences. The effectiveness of clinically-oriented learning approaches is well documented (4, 6).
Against this background, this study was undertaken to assess the knowledge of and attitudes to medical ethics among undergraduate students along with a comparison of the scores of students at different levels of seniority in the college.
Materials and methods
Study design and participants
A descriptive cross-sectional study was carried out from July to November 2009 among the medical undergraduates of different batches, from second year MBBS to the final year, of a medical college in West Bengal, India. First year students were excluded as they have no clinical experience. Institutional ethics committee (IEC) clearance was applied for and obtained. All students of the selected years were briefed on the study’s purpose, and requested to participate in it. The researchers distributed questionnaires after describing the purpose of the study. Students were assured that participation was voluntary, and confidentiality would be maintained. Informed verbal consent was taken from those who chose to participate. Non-respondents were contacted after a 15-day interval, with a repeat request to participate. Of 371 enrolled students, 340 students eventually completed the study – a response rate of 91%. 18 questionnaires were found to be incomplete and were therefore excluded. The final analysis covered 322 students.
A self-administered, semi-structured questionnaire was devised, based on previous research studies and in consultation with faculty members of the department of forensic and state medicine. Some questions were also derived from the code of medical ethics as laid down by the West Bengal Medical Council. The questionnaire was pre-tested on six undergraduate students and the necessary modifications were incorporated into the final questionnaire. The first section of the questionnaire covered demographic information like age, sex, and year of study. The second part of the questionnaire (Tables 1-4) contained questions about their awareness of ethics and its importance, and the source of this awareness; their knowledge of the existence of the ethics committee and its role; their attitudes on various issues such as consent and confidentiality ,privacy; euthanasia , intimate examinationn and their knowledge of the code of medical ethics of the West Bengal Medical Council. The questionnaire did not include information identifying participants.
Data analysis
The collected data was analysed by proportions, bar diagrams, and mean score with 95% confidence interval. Attitudinal questions included a range of response options in accordance with Likert’s 5 point scale (strongly agree, agree, uncertain, disagree, strongly disagree). The responses to each question were given a score, with the most desirable response receiving a high number. The most desirable response for each statement was decided by experts of forensic medicine and also from a literature study. After consultation with a statistical expert, each student’s total scores were categorised as follows: 71 or more out of the maximum possible score of 90 was “very good”, 61-70 was “good”, 51-60 was “fair”, and below 50 was categorised as “poor”.
Results
Among the 322 participants whose responses were analysed, 76% were male and 24% were female. Their ages ranged from 18 to 29 years, with a median age of 22 years.
Table 1 describes the students’ attitude to medical ethics and the source of their information on this. 31.1% were positive about the importance of ethics. 36.8% of fourth year and 31.6% of final year students opined that ethics was “extremely important”. However, four students, including one final year student, thought that such knowledge was “not important”.
Lectures [54.7%] and books on ethics [47.8%] were considered the predominant sources of knowledge. 14.3% participants felt seminars, workshops and clinical training were the most important sources of ethics. Overall, only 10.9% of the respondents had knowledge of the existence of the institutional ethics committee; 21.5% of third year students were aware of this. 22.8% of final year students stated that there was no such committee. 35 students knew of the existence of the IEC. Of these, 9 (25.7%) said its role was to sanction research work; 15 (42.8%) did not know its precise role (not given in table).
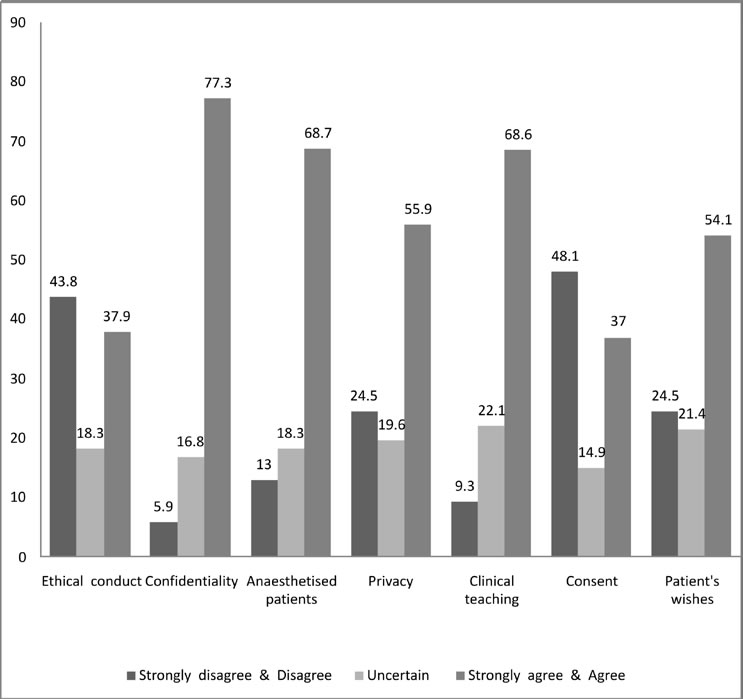
Figure 1 shows that 37.8% agreed and 18.3% were uncertain as to whether “Ethical conduct is important only to avoid legal action.” 68.6% agreed with the statement: “During clinical rounds along with clinical aspects of a patient’s care, it is also essential to discuss ethical, social and legal issues of that patient.” 54% students agreed that “During treatment , the patient’s wishes must always be adhered to.” On the other hand 64.3% students opined that “The doctor should do what is best irrespective of the patient’s opinion.” 73% students will tell the patients “if something goes wrong” and 86% will tell the truth to “close relatives”. 82.6% agreed that “Children (except in emergency) should never be treated without the consent of their parents or guardian.”
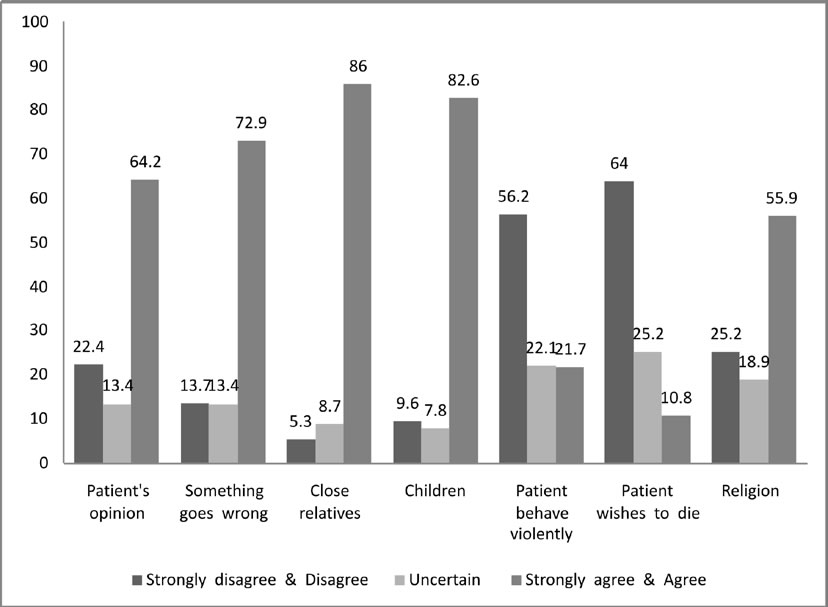
Figure 2 shows that 22% students were uncertain while dealing with “patients who behave violently” and 64% disagreed to the suggestion of euthanasia. 55.9% agreed they will refer the patient to another doctor for religious conflict situations. A majority (77.3%) expressed their commitment to take “informed consent and maintain confidentiality” while doing intimate examinations of patients and 68.6% also agreed that it should be followed even for “anaesthetised or sedated patients”. 55.9% agreed that “Privacy of one patient may be ignored for the benefit of the larger group (i.e. using patient as teaching aid)”.
Table 2 shows that the mean attitude scores of the different batches exploring different areas of ethical issues in everyday practice did not increase correspondingly with increasing years of medical study; in fact, second year students had a better mean total score [3.39; 95%CI ±0.29) than the third year [3.23; 95%CI ± 0.26] fourth year [3.36; 95%CI ± 0.28] or final year [3.37 95%CI ± 0.30].
Table 3 shows that second year students have a better mean score in responses related to the importance of receiving “informed consent for carrying out intimate examination of anaesthetised patients” and whether “privacy of one patient may be ignored for the benefit of the larger group”. The total mean scores of second year [3.77; 95%CI ± 0.27] and third year [4.16; 95% CI ± 0.28] students were found to be better than those of fourth year students [3.67; 95%CI ± 0.31] and those in their final year [3.56; 95%CI ± 0.34].
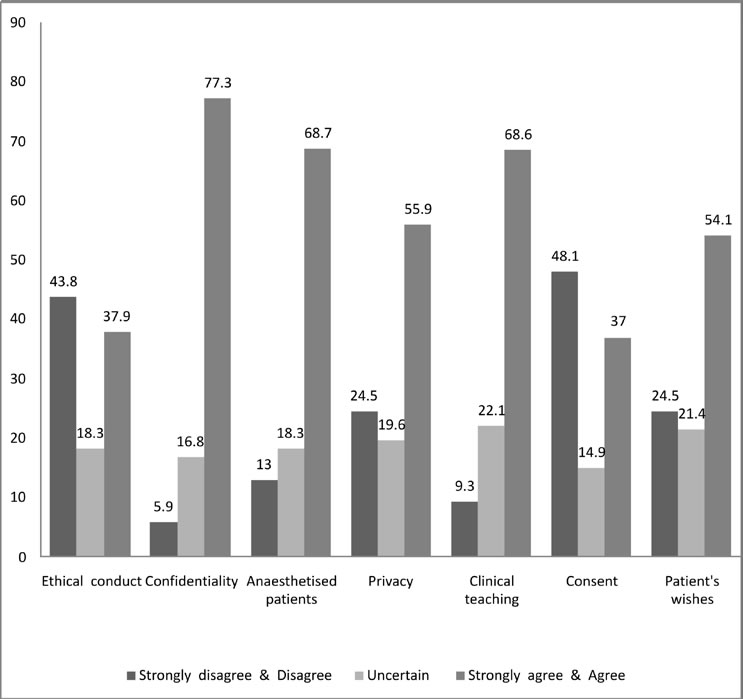
Table 4 describes the students’ knowledge of the code of conduct of the West Bengal Medical Council, to be followed once they graduated. In answer to questions on whether physicians can print their photographs along with qualifications on a signboard and whether they can run shops to dispense drugs or appliances prescribed by other doctors, the mean score was higher than for the other issues. Figure 3 shows that 52.2% disagreed that it was appropriate for doctors to print their photograph on their signboard. 46.3% disagreed that doctors can “run an open shop for dispensing drugs and appliances prescribed by other doctors”. 59.9% agreed that it was better to prescribe drugs by their brand name rather than the generic name and 70.5% agreed that doctors should conduct laboratory investigations even in clinically confirmed cases. 38.8% disagreed that it was necessary for a doctor to retain a copy of the certificate issued by him or her.
The total achieved score (Table 5) shows that only half of the respondent students had a “good” score [61 – 70)], in which the proportion of final year students was low, and 37.26% students achieved a “fair” score [51 – 60].
Discussion
Ethical conflicts are common during the initial years of a medical professional’s career which makes the inculcation of a sound foundation in medical ethics essential. The response rate in the present study was 91%; therefore the results can be considered as representative of the awareness and opinions of medical students of Midnapore Medical College at the time that this study was conducted.
The majority of students knew the importance of medical ethics in their professional life, as in the study done by Walrond E Ret al at the Cave Hill Campus in Barbados in 2003 (7) . However, 4% of the respondent students, including one final year student, thought that it was not important. The study by Shi razet al (8) of surgical team members in Karachi, in 2004, had found that only 3.96% of surgeons did not consider the teaching of ethics at the undergraduate level to be necessary. Another study (4) by Hariharan and others showed that 52% of senior medical staff and 20% of senior nursing staff at their institution in Barbados knew little of the laws pertaining to their work.
The main sources of ethics knowledge as quoted by the study population were classroom lectures [54.7%] and books on ethics [47.8%], as part of forensic medicine. This finding is similar to that in previously completed studies (6, 8).
A study by L W Roberts (1) in 2004 among medical students at a New Mexico school found that respondents preferred clinical and expert-oriented learning like case conferences, and workshops involving a multidisciplinary approach over the traditional didactic approach which was also shown as significantly [p < 0.0001] effective. Discussion by multidisciplinary experts, of experiences in the field, may be helpful to train ethically competent doctors.
Only 10.9% of the students were aware of the existence of the institutional ethics committee and many of them did not know its specific functions. This highlights the need for the administrative section of teaching hospitals to publicise their work at regular intervals for the benefit of trainees. The institutional ethics committee should publish reports related to its involvement in different health-related activities within the institution, and these should be circulated among the students as well.
Students were not very clear about whether “ethical conduct is only important to avoid legal action”. Students often expressed contradictory views in different areas of ethical issues e.g.- while dealing with treatment of patients, most students agreed to adhering to “patient’s wishes”, on the other hand nearly 2/3rd of the students opined that “doctor should do what is best” ignoring the patient’s opinion. Similarly, while undertaking an intimate examination the majority committed to “maintain confidentiality”. At the same time most students said that the privacy of one patient may be ignored for the benefit of teaching purposes. Reasons for this could not be explained properly, but perhaps the students were more interested in developing their clinical acumen rather than in ethics. In some other areas like treating “children”, taking “informed consent”, telling the truth about the worsening condition of patients to “close relatives”, a majority understood the issues. More students disagreed with the statement that physicians must aid patients who wish to die, regardless of the illness. This too, is similar to the findings shown in the study by Walrond, Jonnalagadda, Hariharan and Moseley (7). Regarding medical students’ awareness of the West Bengal Medical Council’s code of conduct, to be followed in their future professional life, the students’ responses revealed an awareness of some aspects of ethics, but a lack of it in others.
A comparison of the mean scores of respondents studying in different years, exploring various ethical issues, shows that there is no proportionate increase in awareness of ethical issues along with an increase in the years of medical education; the mean score of second year students was better than that of their seniors This, too, was similar to the findings in other studies (1, 6). This suggests that the mode of teaching, predominantly didactic and text book-oriented, does not increase students’ awareness of this subject. Clinically-oriented approaches with interactive components through case studies and workshops may be more effective.
The situation does not appear to improve once medical education is completed, and it may even worsen as trainees progress through education, as shown by many studies (9, 10). A three-year cohort study by Patenaude and others (6) at the University of Sherbrooke Medical School in Quebec, Canada, found that students’ understanding of ethics did not improve substantially with education. 72% of the students surveyed remained at the same stage of moral reasoning in their third year of study as in their first, as evidenced by mean scores of 3.46 in the first year and 3.48 in the third year. In fact, 13% moved down to the lower stage and only 15% moved to the higher stage.. The mean attitude score in relation to the intimate examination of patients to adhere to rules regarding informed consent and confidentiality also showed that second and third year students had higher mean scores than their seniors.
Overall, the study revealed that 50.9% had a ‘good’ score [61-70]. 37.3% students had a ‘fair’ score [51-60].All the above findings of this study emphasise the importance of continuing ethics education throughout the undergraduate, internship, and postgraduate periods. Registered professional organisations like the Indian Medical Association and the Indian Public Health Association should provide detailed guidelines on medical ethics in their journals, to prepare future generations of medical professionals for ethically sound practice.
Conclusion
This study highlights the lack of improvement in ethics awareness corresponding to increasing exposure to medical education over four years. It is important to gather baseline information on ethics awareness from different batches of students to guide the evaluation of the current ethics curriculum along with its teaching methodology. To strengthen ethical reasoning and judgment in decision making, clinically oriented pedagogical measures like case studies, seminars, interactive workshops, utilising the work experience of multidisciplinary medical expertise, is needed. This should be an ongoing process, akin to continuing medical education.
Acknowledgements
We thank the Indian Council of Medical Research which funded this research studentship.
| Table 1 : Medical students according to their knowledge of medical ethics | |||||
| Knowledge | 2ND year (n=80) no(%) | 3RD year (n=79) no(%) | 4TH year (n=84) no(%) | Final year (n=79) no(%) | Total (n=322) no(%) |
| How important are ethical issues in your profession? | |||||
| Not at all | 8 (10) | 2 (2.5) | 2 (2.4) | 1 (1.3) | 13 (4.4) |
| Somewhat important | 2 (15) | 11 (13.9) | 12 (14.3) | 5 (6.2) | 40 (12.3 |
| Important | 28 (35) | 28 (35.4) | 16 (19.1) | 19 (24.1) | 91 (28.2) |
| Very important | 20 (25) | 28 (35.4) | 23 (27.4) | 29 (36.7) | 100 (31.1 |
| Extremely important | 12 (15) | 10 (12.8) | 31 (36.8) | 25 (31.6) | 78 (24.1) |
| What are the sources of your knowledge? | |||||
| Lecture classes | 23 (28.8) | 52 (65.82) | 54 (64.3) | 47 (59.5) | 176 (54.7) |
| Ethical Books | 19 (23.8) | 38 (48.1) | 46 (54.8) | 51 (64.6) | 154 (47.8) |
| Seminar & Workshops | 18 (22.5) | 9 (11.4) | 7 (8.3) | 9 (11.4) | 43 (14.3) |
| Clinical Training | 9 (11.3) | 14 (17.7) | 9 (10.7) | 11 (13.9) | 43 (14.3) |
| Journals | 14 (17.5) | 7 (8.9) | 7 (8.3) | 8 (10.1 | 36 (11.2) |
| Newspaper | 37 (46.3) | 25 (31.7) | 24 (28.6) | 18 (22.8) | 104 (32.3) |
| Television | 31 (38.8) | 22 (27.5) | 26 (32.5) | 17 (21.3) | 96 (29.8) |
| Is there an ethics committee in your institution? | |||||
| Yes | 1 (1.3) | 17 (21.5) | 9 (10.7) | 8 (10.1 | 35 (10.9) |
| No | 13 (16.3) | 14 (17.7) | 16 (19.1) | 18 (22.8) | 61 (18.9) |
| Don’t know | 66 (82.4) | 48 (60.8) | 59 (70.2) | 53 (67.1) | 226 (70.2) |
| Table 2 : Comparison of attitude scores of different years of students | ||||||||
| Statements on ethical issues | 2nd yearMean(95%CI) | 3rd yearMean (95%CI) | 4th year Mean (95%CI) | Final year Mean (95%CI ) | ||||
| a) | Ethical conduct is important only to avoid legal action. | 3.13(±0.27) | 2.91(±0.21) | 2.95 (±0.28) | 3.24(±0.29) | |||
| b) | During clinical rounds along with clinical aspects of a patient’s care, it is also essential to discuss ethical , social and legal issues of that patient. | 4.06(±0.19) | 3.36(±0.22) | 3.90(±0.21) | 3.97(±0.20) | |||
| c) | During treatment , the patient’s wishes must always be adhered to. | 2.33(±0.24) | 2.63(±0.19) | 2.67(±0.25) | 2.69(±0.26) | |||
| d) | The doctor should do what is best irrespective of the patient’s opinion. | 3.91(±0.25) | 3.41(±0.26) | 3.64(±0.25) | 3.72(±0.28) | |||
| e) | The patient should always be told if something goes wrong. | 2.03(±0.22) | 2.07(±0.24) | 2.10(±0.22) | 1.94(±0.27) | |||
| f) | Close relatives must always be told about the patient’s condition. | 4.52(±0.17) | 4.13(±0.19) | 4.28(±0.18) | 4.36(±0.22) | |||
| g) | Children (except in emergency) should never be treated without the consentof their parents or guardian. | 4.46(±0.16) | 4.06(±0.24) | 4.01(±0.21) | 3.94(±0.24) | |||
| h) | Doctors and nurses should refuse to treat patients who behave violently. | 3.34(±0.22) | 3.35(±0.23) | 3.27(±0.26) | 3.48(±0.27) | |||
| i) | A patient who wishes to die should be assisted in doing so , no matter whathis/her illness. | 3.72(±0.22) | 3.88(±0.21) | 3.79(±0.25) | 3.81(±0.26) | |||
| j) | Patients who refuse to be treated on religious or other grounds, should betold that they need to find another doctor with their beliefs or accept the treatment offered. | 2.49(±0.26) | 2.16(±0.21) | 2.95(±0.27) | 2.56(±0.27) | |||
| Total | 3.39(± 0.29) | 3.23(±0.26) | 3.36(±0.28) | 3.37(±0.30) | ||||
| Table 3 : Comparison of respondents’ attitude scores regarding intimate examination of patients | ||||
| Intimateexaminationof patients | 2nd year ( n = 80) Mean (95%CI ) | 3rd year (n = 79) Mean(95%CI ) | 4th year (n= 84) Mean (95%CI ) | Final year (n = 79) Mean (95%CI ) |
| a) During clinical teaching it is important to follow certain guidelines for intimate(vaginal , rectal) examinations of the patients like informed consent, maintainconfidentiality | 4.28(±0.25) | 4.16(±0.28) | 4.66(±0.21) | 4.59 (±0.24) |
| b) This should be followed even for anaesthetised or sedated patients | 4.13(±0.18) | 3.78(±0.23) | 3.8(±0.27) | 3.7(±0.29) |
| c ) Privacy of one patient may be ignored for the benefit of the larger group | 2.91(±0.28) | 2.51(±0.22) | 2.52(±0.27) | 2.35(±0.28) |
| Total | 3.77(± 0.27) | 4.16(±0.28) | 3.67(±0.31) | 3.56(±0.34) |
| Table 4 : Knowledge of the code of conduct of the West Bengal Medical Council | ||||
| Statement ofacceptablebehaviour | 2nd Year ( n = 80) Mean(95%CI ) | 3rd Year (n = 79) Mean (95%CI ) | 4th Year (n= 84) Mean (95%CI ) | Final Year (n = 79) Mean (95%CI ) |
| a) A physician may print his or her photograph n the signboard, along withqualification and speciality | 3.2 (±0.28) | 3.07 (±0.26) | 3.63 (±0.25) | 3.22 (±0.29) |
| b) A physician may run an open shop for dispensing drugs and appliancesprescribed by other doctors | 2.95 (±0.26) | 3.13 (±0.24) | 3.60 (±0.26) | 3.49 (±0.26) |
| c) In one’s practice it is better to use the brand name than the generic name of adrug | 2.58 (±0.28) | 2.27 (±0.24) | 2.92 (±0.29) | 2.50 (±0.28) |
| d) Clinically confirmed cases should also undergo laboratory investigations as aroutine | 2.01 (±0.17) | 2.27 (±0.19) | 2.34 (±0.25) | 2.29 (±0.26) |
| e) It is not always necessary for a physician to keep a copy of the certificate issuedby him or her | 2.98 (±0.25) | 2.87 (±0.28) | 2.94 (±0.27) | 2.59 (±0.27) |
| Total | 2.74 (± 0.27) | 2.72 (±0.26) | 3.09 (±0.28) | 2.82 (±0.29) |
| Table 5 : Total scores on medical ethics obtained by students in different years | |||||
| Grading of score | 2nd year(n=80)no(%) | 3rd year(n=79) no(%) | 4th year(n=84) no(%) | Final year(n=79) no (%) | Total(n=322) no(%) |
| Poor(≤ 50) | 1(1.3) | 7(8.90 | 0(0) | 4(5.1) | 12(3.7) |
| Fair (51-60) | 28(35) | 31(39.2) | 31(36.9) | 30(38) | 120(37.3) |
| Good (61-70) | 46(57.4) | 40(50.7) | 45(53.6) | 33(41.7) | 164(50.9) |
| Very good (≥ 71) | 5(6.3) | 1(1.2) | 8(9.5) | 12(15.2) | 26(8.1) |
References
- Roberts LW, Green Hammond KA, Geppert GM, Warner TD. The positive role of professionalism and ethics training in medical education: a comparison of medical student and resident perspectives. Acad Psychiatry. 2004 Fall; 28(3):170-82.
- Sulmasy D P, Geller G, Levine DM, Faden R R. A randomized trial of ethics education for medical house officers. J Med Ethics. 1993 Sep; 19(3): 157-63.
- Elger BS, Harding T W. Terminally ill patients and Jehovah’s Witnesses : teaching acceptance of patients’ refusals of vital treatments. Med Educ. 2002 May; 36(5): 479-88.
- Hariharan S, Jonnalagadda R, Walrond E and Moseley H. Knowledge, attitude and practice of health care ethics and law among doctors and nurses in Barbados. BMC Med Ethics.2006 Jun; 9;7:E7
- Yacoub AA, Ajeel NA. Teaching medical ethics in Basra: perspective of students and graduates. East Mediterr Health J. 2000 Jul;6(4):687-92.
- Patenaude J, Niyonsenga T, Fafard D. Changes in students’ moral development during medical school: a cohort study. CMAJ. 2003 Apr1;168(7):840-4.
- Walrond ER, Jonnalagadda R, Hariharan S, Moseley HS. Knowledge, attitudes and practice of medical students at the Cave Hill Campus in relation to ethics and law in healthcare.West Indian Med J. 2006 Jan; 55(1): 42-7.
- Shiraz B, Shamim MS, Shamim MS, Ahmed A. Medical ethics in surgical words: knowledge, attitude and practice of surgical team members in Karachi. Indian J Med Ethics.2005 Jul-Sep;2(3);94-6.
- Hicks LK, Lin Y, Robertson DW, Robinson DL, Woodrow Sl. Understanding the clinical dilemmas that shape medical students’ ethical development: questionnaire survey and focus group study. BMJ. 2001Mar. 24;322(7288):709-10.
- Feudtner C, Christakis DA. Ethics in a short white coat: the ethical dilemmas that medical students confront. Acad Med. 1993 Apr; 68(4):249-54.